Gastrointestinal bleeding represents one of the most concerning digestive health issues that can affect people of all ages. This condition occurs when blood loss happens anywhere along the digestive tract, from the mouth to the anus, and can range from minor episodes to life-threatening medical emergencies.
Whether you're experiencing symptoms yourself or seeking information for a loved one, understanding the warning signs, causes, and treatment approaches for gastrointestinal bleeding is crucial for making informed healthcare decisions and knowing when to seek immediate medical attention.
What Is Gastrointestinal Bleeding?
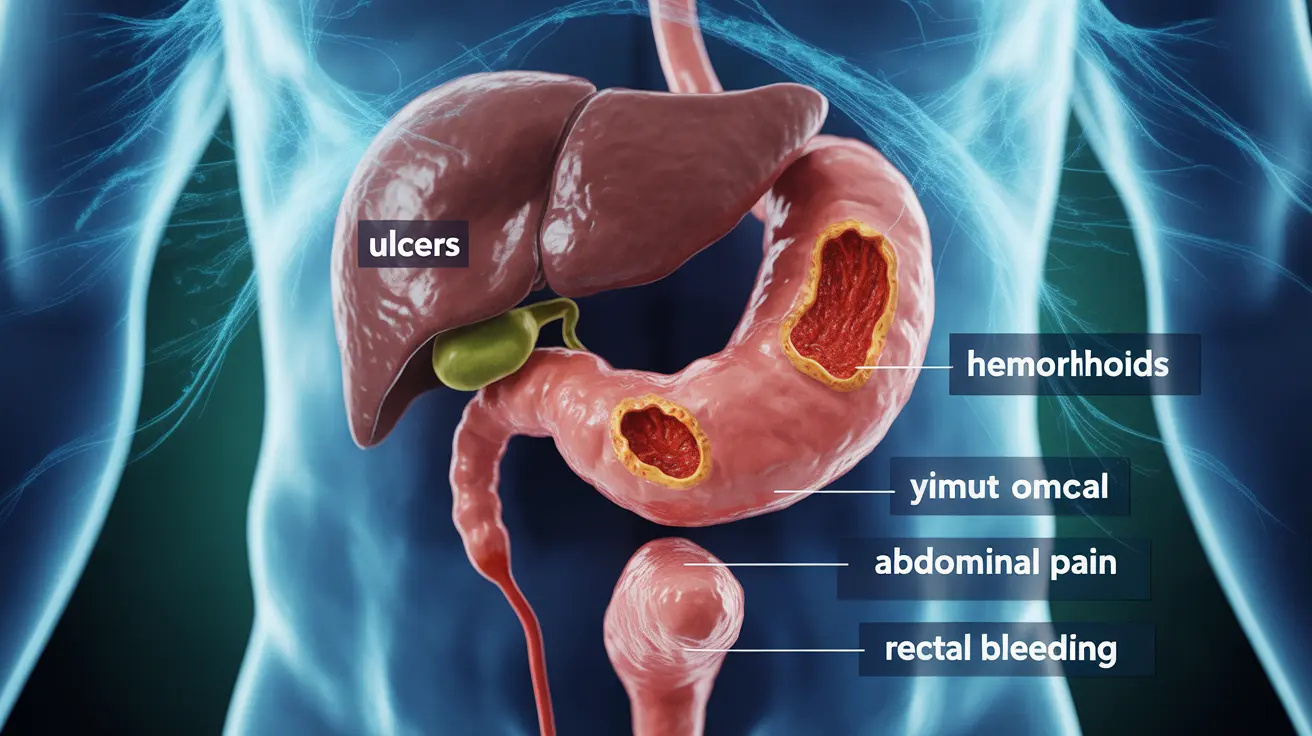
Gastrointestinal bleeding occurs when there is blood loss from any part of the digestive system, including the esophagus, stomach, small intestine, large intestine, rectum, or anus. Medical professionals typically classify this condition into two main categories: upper gastrointestinal bleeding, which affects areas above the small intestine, and lower gastrointestinal bleeding, which involves the colon and rectum.
The severity of gastrointestinal bleeding can vary dramatically. Some people experience slow, chronic bleeding that may go unnoticed for weeks or months, while others face acute episodes requiring immediate emergency care. The underlying cause, location, and rate of bleeding all influence the symptoms and urgency of treatment needed.
Common Causes of Gastrointestinal Bleeding
Upper Gastrointestinal Causes
Peptic ulcers rank among the most frequent causes of upper gastrointestinal bleeding. These painful sores develop in the stomach lining or the first part of the small intestine, often due to infection with Helicobacter pylori bacteria or prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs). When these ulcers erode deeply enough, they can damage blood vessels and cause bleeding.
Esophageal varices present another serious cause, particularly in individuals with liver disease or cirrhosis. These enlarged veins in the esophagus can rupture and cause severe bleeding. Additionally, tears in the esophageal lining, known as Mallory-Weiss tears, can occur from violent vomiting or retching.
Lower Gastrointestinal Causes
Hemorrhoids represent the most common cause of lower gastrointestinal bleeding, especially in adults over 50. These swollen blood vessels in the rectum and anus can bleed during bowel movements, typically producing bright red blood. Anal fissures, which are small tears in the anal tissue, can also cause similar bleeding patterns.
Diverticular disease affects many older adults and can lead to bleeding when small pouches in the colon wall become inflamed or infected. Inflammatory bowel diseases, including Crohn's disease and ulcerative colitis, can cause chronic bleeding along with other digestive symptoms.
Recognizing the Symptoms
The symptoms of gastrointestinal bleeding depend largely on the location, severity, and duration of the bleeding. Upper gastrointestinal bleeding often presents with vomiting blood, which may appear bright red or look like coffee grounds. Patients may also experience black, tarry stools called melena, which occur when blood from the upper digestive tract is digested and darkened.
Lower gastrointestinal bleeding typically produces bright red blood in the stool or blood mixed with bowel movements. Some people notice blood on toilet paper after wiping or see drops of blood in the toilet bowl. In cases of severe bleeding, patients may experience dizziness, weakness, rapid heartbeat, or fainting due to blood loss and resulting anemia.
Chronic, slow bleeding may cause more subtle symptoms such as fatigue, shortness of breath, pale skin, or unexplained weakness. These signs often develop gradually as the body's iron stores become depleted, leading to iron-deficiency anemia.
Diagnostic Approaches and Treatment Methods
Medical Evaluation
Healthcare providers use various diagnostic tools to identify the source and severity of gastrointestinal bleeding. Initial assessment typically includes a thorough medical history, physical examination, and blood tests to check for anemia and clotting disorders. Complete blood count tests help determine the extent of blood loss and guide treatment decisions.
Endoscopic procedures play a crucial role in diagnosing gastrointestinal bleeding. Upper endoscopy allows doctors to examine the esophagus, stomach, and upper small intestine using a flexible camera, while colonoscopy provides visualization of the large intestine. These procedures not only help identify bleeding sources but can also provide therapeutic interventions.
Treatment Strategies
Treatment approaches for gastrointestinal bleeding vary significantly based on the underlying cause and severity. For peptic ulcers, doctors may prescribe proton pump inhibitors to reduce stomach acid production and antibiotics to eliminate H. pylori bacteria. Endoscopic interventions can directly treat bleeding ulcers through cauterization or injection of clotting agents.
Minor bleeding from hemorrhoids or anal fissures may respond well to conservative treatments such as high-fiber diets, stool softeners, and topical medications. More severe cases might require surgical interventions or minimally invasive procedures to address the bleeding source.
In cases of severe acute bleeding, patients may need blood transfusions, intravenous fluids, and intensive monitoring. Emergency surgery becomes necessary when bleeding cannot be controlled through less invasive means or when complications arise.
Prevention and Long-Term Management
Preventing gastrointestinal bleeding often focuses on addressing modifiable risk factors and maintaining digestive health. Limiting or avoiding NSAIDs can significantly reduce the risk of peptic ulcers, especially in older adults or those with a history of stomach problems. When these medications are necessary, doctors may recommend concurrent use of stomach-protecting drugs.
Dietary modifications can play an important role in prevention. Consuming a high-fiber diet helps maintain healthy bowel movements and may reduce the risk of hemorrhoids and diverticular disease. Limiting alcohol consumption is particularly important for individuals with liver disease or at risk of developing esophageal varices.
Regular medical check-ups and appropriate screening tests can help identify and address potential bleeding sources before they become serious problems. Individuals with inflammatory bowel disease or other chronic digestive conditions benefit from ongoing medical management and monitoring.
Frequently Asked Questions
What are the most common causes and symptoms of gastrointestinal bleeding?
The most common causes include peptic ulcers, hemorrhoids, esophageal varices, and inflammatory bowel disease. Symptoms vary by location but may include vomiting blood, black tarry stools, bright red blood in stool, abdominal pain, weakness, dizziness, and signs of anemia such as fatigue and pale skin.
How is gastrointestinal bleeding diagnosed and what treatments are available?
Diagnosis involves blood tests, physical examination, and endoscopic procedures like upper endoscopy or colonoscopy. Treatments range from medications such as proton pump inhibitors and antibiotics for ulcers, to endoscopic interventions, surgical procedures, blood transfusions, and supportive care depending on the cause and severity.
What can I do at home to help manage or stop minor gastrointestinal bleeding?
For minor bleeding, increase fiber intake, stay hydrated, avoid NSAIDs and alcohol, and use stool softeners if constipated. However, any gastrointestinal bleeding should be evaluated by a healthcare provider, as home remedies cannot address underlying causes and may delay necessary medical treatment.
When should I seek emergency medical attention for gastrointestinal bleeding?
Seek immediate emergency care if you experience vomiting large amounts of blood, severe abdominal pain, dizziness or fainting, rapid heartbeat, difficulty breathing, confusion, or signs of severe blood loss. Any significant change in bleeding patterns or new onset of bleeding symptoms warrants prompt medical evaluation.
What lifestyle changes or medications can help prevent gastrointestinal bleeding from happening again?
Prevention strategies include avoiding NSAIDs when possible, limiting alcohol consumption, maintaining a high-fiber diet, managing stress, treating H. pylori infections, and following prescribed medications for underlying conditions. Regular medical follow-ups and adherence to treatment plans for chronic digestive diseases are essential for preventing recurrence.