Many people are surprised to learn that gastroesophageal reflux disease (GERD) can cause breathing difficulties, including shortness of breath. This connection between digestive and respiratory symptoms often leads to confusion and concern among those experiencing both issues. Understanding how GERD affects breathing is crucial for proper diagnosis and treatment.
In this comprehensive guide, we'll explore the relationship between GERD and respiratory symptoms, helping you understand when to seek medical attention and what treatment options are available.
How GERD Affects Your Breathing
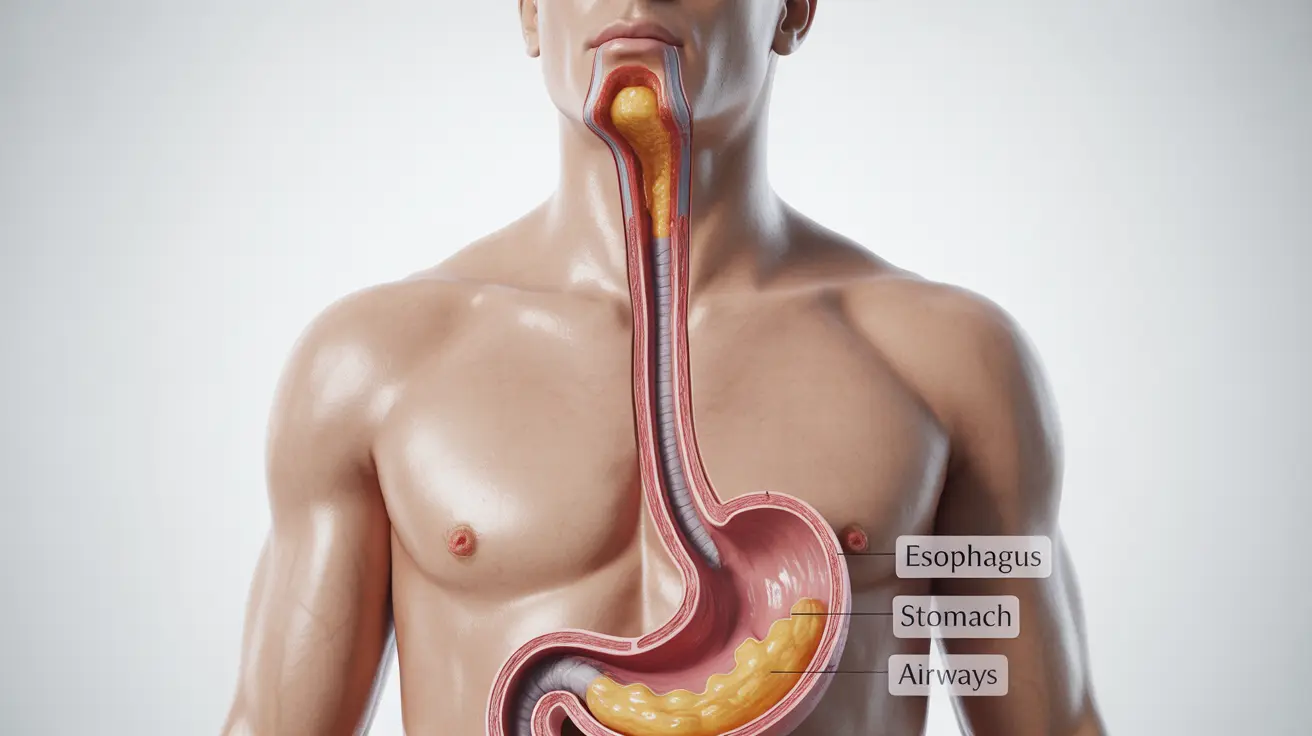
When stomach acid flows back into the esophagus, it can trigger a series of reactions that affect your respiratory system. The acid reflux can cause inflammation and irritation in the airways, leading to breathing difficulties. Additionally, micro-aspirations of stomach contents can irritate the lungs and bronchial tubes, potentially causing shortness of breath.
Common Respiratory Symptoms
GERD can manifest through various respiratory symptoms, including:
- Wheezing
- Chronic cough
- Chest tightness
- Difficulty taking deep breaths
- Recurring bronchitis
- Voice changes or hoarseness
The GERD-Asthma Connection
Research has shown a strong link between GERD and asthma, with each condition potentially worsening the other. When acid reflux irritates the airways, it can trigger asthma symptoms or make existing asthma more severe. Conversely, asthma-related chest pressure can weaken the lower esophageal sphincter, leading to more frequent acid reflux episodes.
Diagnosing GERD-Related Breathing Issues
Healthcare providers use several methods to determine if shortness of breath is related to GERD:
- pH monitoring tests
- Endoscopy
- Pulmonary function tests
- Chest X-rays
- Esophageal manometry
Treatment Options and Management Strategies
Managing GERD-related breathing difficulties typically involves a multi-faceted approach:
Medication Options
Several medications can help control GERD symptoms and related breathing issues:
- Proton pump inhibitors (PPIs)
- H2 blockers
- Antacids
- Bronchodilators (if asthma is present)
Lifestyle Changes
Making certain lifestyle modifications can significantly improve both GERD and breathing symptoms:
- Elevating the head of the bed
- Avoiding meals close to bedtime
- Maintaining a healthy weight
- Avoiding trigger foods
- Quitting smoking
- Wearing loose-fitting clothes
Frequently Asked Questions
Can GERD cause shortness of breath and how does acid reflux affect breathing? Yes, GERD can cause shortness of breath through several mechanisms. Acid reflux can irritate the airways and trigger inflammation, leading to breathing difficulties. Additionally, stomach acid can sometimes be aspirated into the lungs, causing direct respiratory symptoms.
What are the common respiratory symptoms linked to GERD besides shortness of breath? Common respiratory symptoms associated with GERD include chronic cough, wheezing, chest tightness, hoarseness, and recurrent bronchitis. Some people may also experience a sensation of something stuck in their throat or difficulty taking deep breaths.
How is shortness of breath caused by GERD diagnosed and differentiated from other lung or heart problems? Doctors use various diagnostic tools including pH monitoring, endoscopy, pulmonary function tests, and chest X-rays to determine if breathing problems are GERD-related. They also carefully evaluate symptoms and medical history to rule out other conditions.
What treatments and lifestyle changes can help reduce shortness of breath caused by GERD? Treatment typically combines medication (such as PPIs or H2 blockers) with lifestyle changes like elevating the head of the bed, avoiding late meals, maintaining a healthy weight, and identifying trigger foods. Some patients may also benefit from stress reduction techniques.
Can acid reflux worsen asthma or cause asthma-like symptoms in people with GERD? Yes, acid reflux can both worsen existing asthma and cause asthma-like symptoms in people with GERD. The relationship is bidirectional, meaning each condition can exacerbate the other, making proper management of both conditions essential.