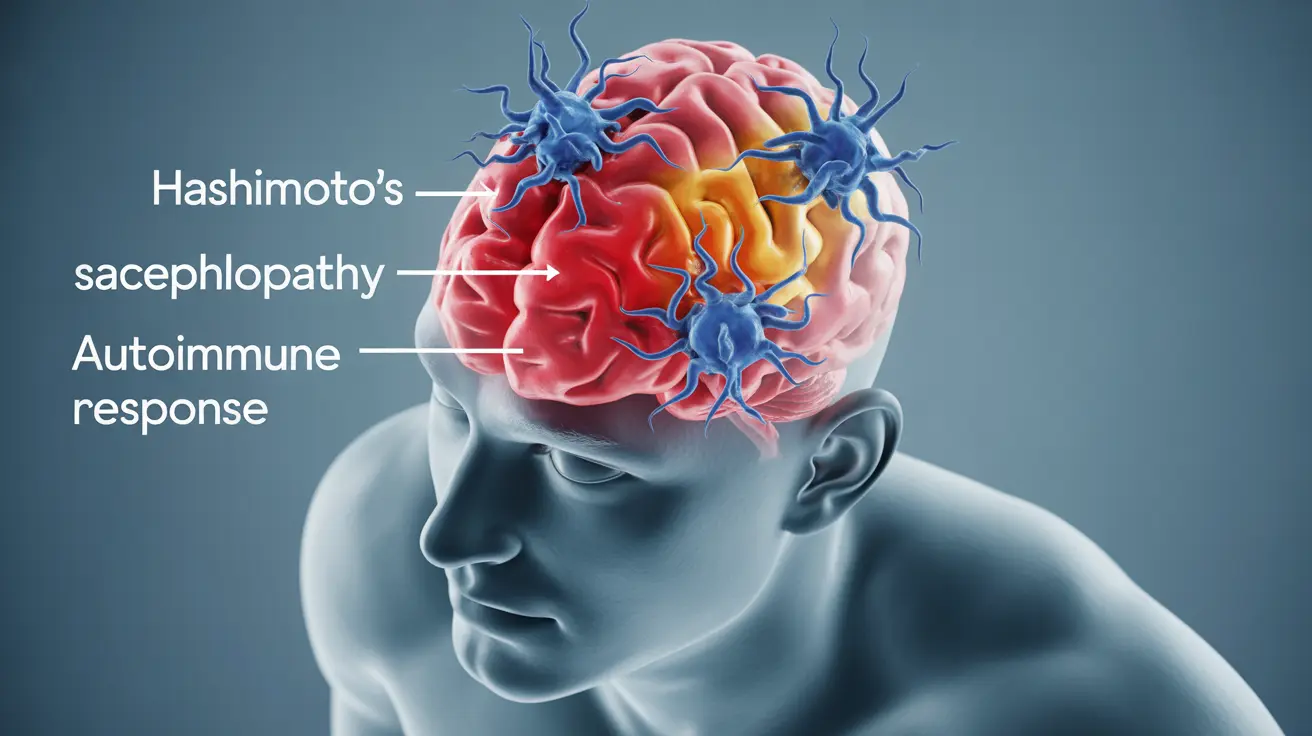
Hashimoto's encephalopathy is a rare but serious neurological condition that can affect brain function and cognitive abilities. This complex disorder, also known as steroid-responsive encephalopathy associated with autoimmune thyroiditis (SREAT), occurs when the immune system mistakenly attacks brain tissue, leading to inflammation and various neurological symptoms.
While the condition shares its name with Hashimoto's thyroiditis, an autoimmune thyroid disorder, the relationship between the two conditions isn't fully understood. Early recognition and proper treatment are crucial for managing symptoms and preventing long-term complications.
Key Symptoms and Brain Effects
Hashimoto's encephalopathy can present with a wide range of neurological and psychiatric symptoms, which often develop gradually over time. Common manifestations include:
- Cognitive decline and confusion
- Seizures and tremors
- Memory problems
- Difficulty with concentration
- Speech difficulties
- Changes in consciousness or personality
- Sleep disturbances
- Coordination problems
These symptoms can significantly impact daily functioning and quality of life, making prompt medical attention essential for anyone experiencing these signs.
Diagnostic Challenges and Approaches
Diagnosing Hashimoto's encephalopathy can be challenging due to its similarity to other neurological conditions. Doctors typically use a combination of diagnostic tools and criteria, including:
- Blood tests for thyroid antibodies
- Neurological examination
- Brain imaging (MRI, CT scans)
- Electroencephalogram (EEG)
- Spinal fluid analysis
- Cognitive function tests
The presence of elevated thyroid antibodies, particularly thyroid peroxidase antibodies (TPO), along with neurological symptoms and response to steroid treatment, often helps confirm the diagnosis.
Treatment Strategies and Management
The primary treatment for Hashimoto's encephalopathy involves immunosuppressive therapy, with corticosteroids being the first-line treatment. Most patients respond well to corticosteroids, showing significant improvement in symptoms within weeks of starting treatment.
First-Line Treatment Options
Typical treatment approaches include:
- High-dose corticosteroids (usually prednisone)
- Gradual dose reduction based on response
- Long-term maintenance therapy when necessary
- Regular monitoring of symptoms and side effects
Alternative Treatments
For patients who don't respond well to corticosteroids or cannot tolerate them, alternative treatments may include:
- Other immunosuppressive medications
- Intravenous immunoglobulin therapy
- Plasmapheresis in severe cases
Long-Term Management and Monitoring
Long-term management of Hashimoto's encephalopathy requires careful monitoring and adjustment of treatment strategies. Regular medical follow-up is essential to:
- Track symptom progression or improvement
- Monitor for potential treatment side effects
- Adjust medication dosages as needed
- Assess overall health status
- Manage any concurrent thyroid conditions
Frequently Asked Questions
1. What are the common symptoms of Hashimoto's encephalopathy and how do they affect the brain? The condition primarily affects cognitive function, causing symptoms like confusion, memory problems, seizures, and personality changes. These symptoms result from brain inflammation and can impact various areas of brain function.
2. How is Hashimoto's encephalopathy diagnosed given its similarity to other neurological conditions? Diagnosis involves a combination of blood tests for thyroid antibodies, neurological examinations, brain imaging, and other diagnostic tests. The key is identifying elevated thyroid antibodies along with neurological symptoms while ruling out other conditions.
3. What treatment options are available for Hashimoto's encephalopathy and how effective are corticosteroids? Corticosteroids are the primary treatment and are typically very effective, with most patients showing significant improvement. Alternative treatments include other immunosuppressive medications and immunoglobulin therapy for those who don't respond to steroids.
4. Can Hashimoto's encephalopathy be safely managed long-term, and what are the risks of immunosuppressive therapy? Long-term management is possible with careful monitoring and appropriate medication adjustments. Risks of immunosuppressive therapy include increased susceptibility to infections, bone density loss, and other potential side effects that require regular medical supervision.
5. When should someone with neurological or psychiatric symptoms seek medical evaluation for possible Hashimoto's encephalopathy? Anyone experiencing unexplained neurological symptoms, particularly cognitive changes, seizures, or personality changes, should seek immediate medical evaluation. Early diagnosis and treatment are crucial for better outcomes.