Hemianopsia, a complex visual condition, affects a person's field of vision by causing partial blindness in one half of the visual field. This condition can significantly impact daily activities and quality of life, making it crucial to understand its nature, causes, and available treatment approaches.
Whether caused by stroke, brain injury, or other neurological conditions, hemianopsia requires proper medical attention and management strategies to help affected individuals maintain their independence and adapt to visual changes.
What is Hemianopsia?
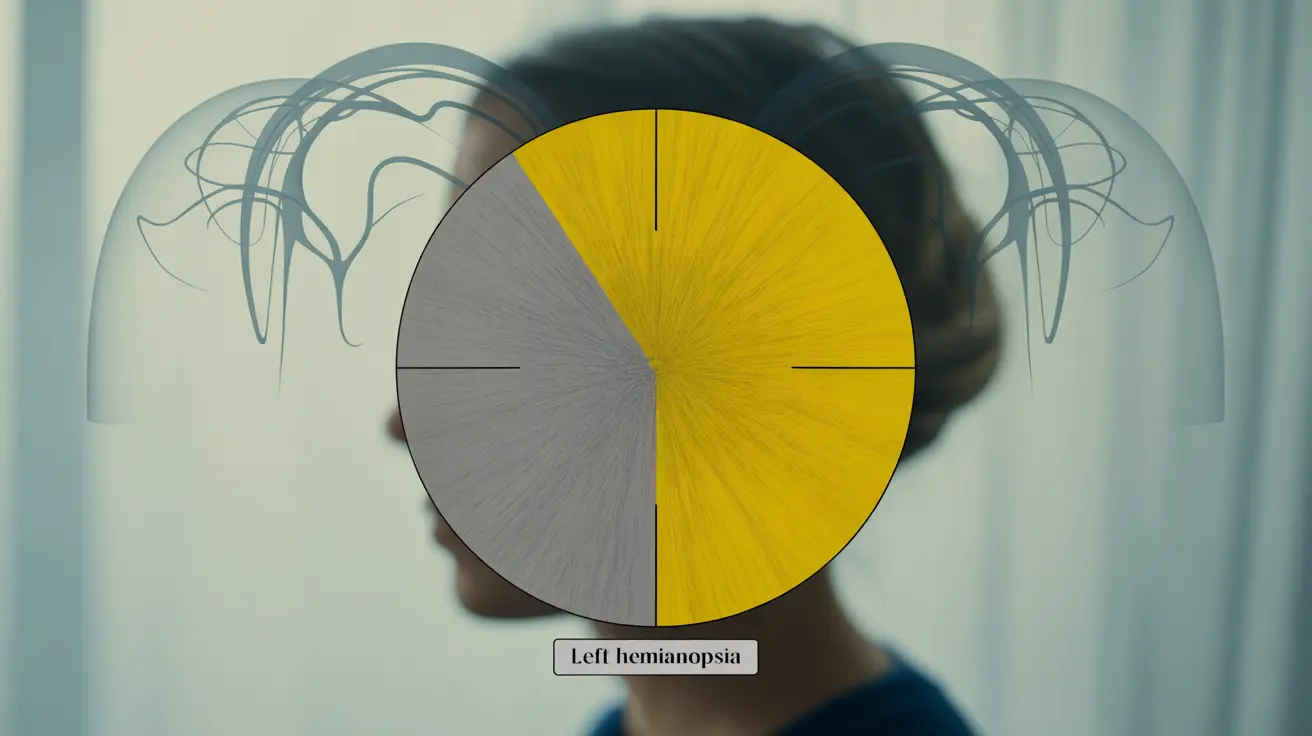
Hemianopsia, also known as hemianopia, occurs when a person loses vision in half of their visual field in one or both eyes. This vision loss follows a specific pattern depending on which part of the brain's visual pathway is affected. The condition can be either homonymous (affecting the same side in both eyes) or heteronymous (affecting opposite sides in each eye).
Types of Hemianopsia
Several distinct types of hemianopsia exist, each with unique characteristics:
- Homonymous hemianopsia: Affects the same side of vision in both eyes
- Bitemporal hemianopsia: Affects the outer field of vision in both eyes
- Binasal hemianopsia: Affects the inner field of vision in both eyes
- Superior hemianopsia: Affects the upper half of the visual field
- Inferior hemianopsia: Affects the lower half of the visual field
Common Causes and Risk Factors
Hemianopsia typically results from damage to the brain's visual pathway. Common causes include:
- Stroke or cerebrovascular accidents
- Traumatic brain injury
- Brain tumors
- Multiple sclerosis
- Surgical complications
- Cerebral aneurysms
- Neurological disorders
Diagnosis Process
Diagnosing hemianopsia involves several specialized tests and examinations:
- Visual field testing
- Neurological examination
- Brain imaging (MRI or CT scans)
- Ophthalmological assessment
- Visual acuity testing
Treatment and Management Strategies
While there's no direct cure for hemianopsia, several treatment approaches can help manage the condition:
Vision Rehabilitation
Vision rehabilitation therapy focuses on helping patients adapt to their visual field loss through specialized exercises and techniques.
Compensatory Strategies
Patients learn specific techniques to compensate for their visual field loss, including:
- Visual scanning exercises
- Head turning techniques
- Environmental modifications
- Use of visual aids and technology
Adaptive Technologies
Various devices and tools can assist patients in daily activities:
- Specialized glasses with prisms
- Vision restoration therapy systems
- Mobile apps for vision training
- Navigation assistance devices
Living with Hemianopsia
Adapting to life with hemianopsia requires patience and proper support. Important considerations include:
- Making home modifications for safety
- Developing new reading strategies
- Learning safe mobility techniques
- Building a strong support network
Frequently Asked Questions
What does hemianopsia mean and how does it affect vision? Hemianopsia refers to the loss of vision in half of the visual field in one or both eyes. It affects vision by creating a blind spot in specific areas of sight, impacting a person's ability to see objects, people, or obstacles in the affected area.
What are the most common causes of hemianopsia? The most common causes of hemianopsia include stroke, traumatic brain injury, brain tumors, and neurological conditions that affect the visual pathway in the brain.
What symptoms should I look for if I suspect hemianopsia? Key symptoms include difficulty seeing objects on one side of the visual field, bumping into objects on the affected side, trouble reading entire lines of text, and challenges with spatial awareness.
How is hemianopsia diagnosed by doctors? Doctors diagnose hemianopsia through comprehensive visual field testing, neurological examinations, brain imaging studies (MRI or CT scans), and detailed eye examinations.
What treatment options and management strategies are available for hemianopsia? Treatment options include vision rehabilitation therapy, compensatory strategy training, adaptive technologies like prism glasses, and specialized exercises to improve visual scanning abilities. While there's no cure, these approaches help patients better manage their condition and maintain independence.