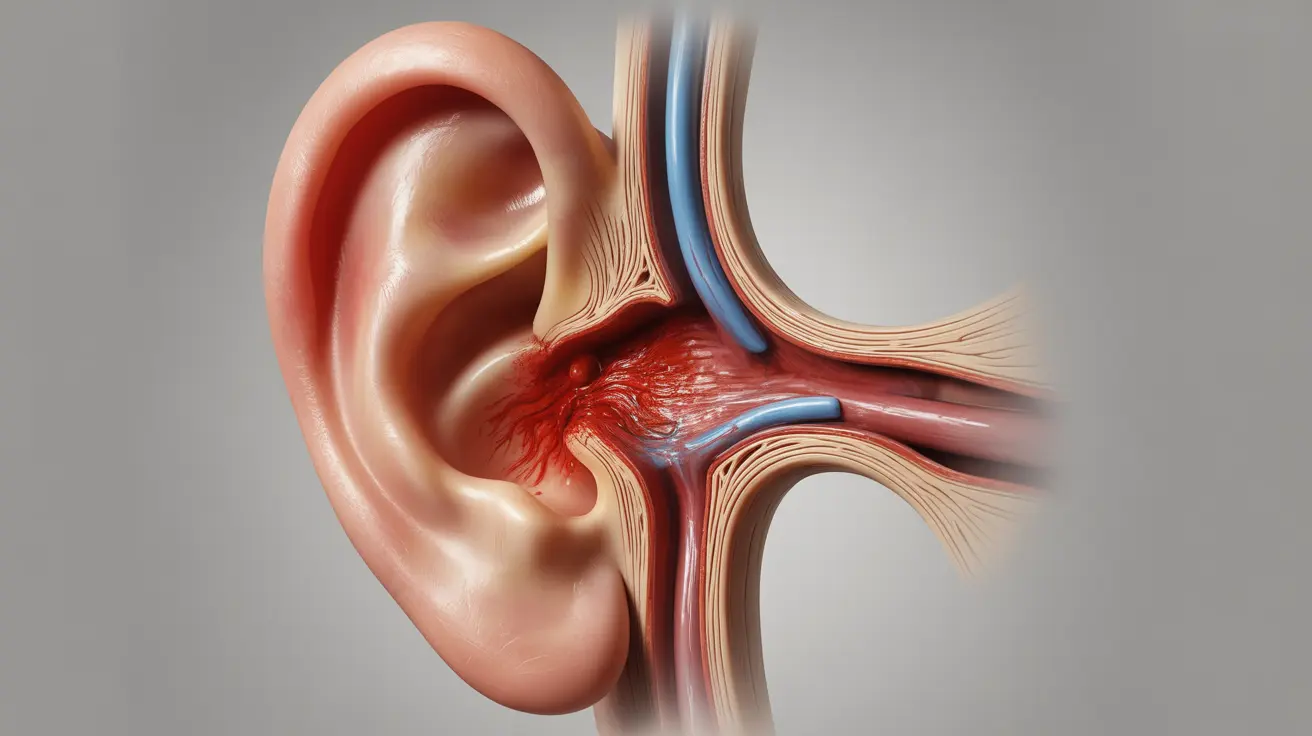
Hemotympanum is a medical condition characterized by blood accumulation behind the eardrum, also known as the tympanic membrane. This condition can occur due to various causes, from trauma to underlying medical conditions, and requires proper medical attention for accurate diagnosis and treatment.
While hemotympanum itself isn't always immediately dangerous, it can signal serious underlying conditions and may lead to hearing complications if left untreated. Understanding its symptoms, causes, and treatment options is crucial for anyone experiencing ear-related issues.
What is Hemotympanum?
Hemotympanum occurs when blood collects in the middle ear space behind the eardrum. This condition can affect people of all ages and may present in one or both ears, depending on the underlying cause. The presence of blood in this space can interfere with normal ear function and sound transmission.
Common Signs and Symptoms
Recognizing the symptoms of hemotympanum is crucial for seeking timely medical attention. Common indicators include:
- Hearing loss or muffled hearing
- Ear fullness or pressure
- Discomfort or pain in the affected ear
- Changes in ear appearance (the eardrum may appear dark or bluish)
- Tinnitus (ringing in the ears)
Causes and Risk Factors
Several factors can lead to the development of hemotympanum:
Trauma-Related Causes
- Head injuries
- Barotrauma (pressure-related injury)
- Skull base fractures
- Direct ear trauma
Medical Conditions
- Blood disorders
- Chronic ear infections
- Tumors in the ear or nearby structures
- Vascular abnormalities
Diagnosis Process
Healthcare providers use various methods to diagnose hemotympanum accurately:
- Otoscopic examination
- Physical examination
- Medical history review
- Imaging studies (when necessary)
- Hearing tests
Treatment Approaches
The treatment of hemotympanum depends largely on its underlying cause and severity. Treatment options may include:
Conservative Management
- Observation and monitoring
- Pain management
- Rest and recovery
Medical Interventions
- Antibiotics (if infection is present)
- Treatment of underlying conditions
- Middle ear fluid drainage (when necessary)
Potential Complications
If left untreated, hemotympanum can lead to several complications:
- Persistent hearing loss
- Chronic ear problems
- Middle ear infections
- Tympanic membrane damage
Prevention Strategies
While not all cases of hemotympanum can be prevented, certain measures can reduce risk:
- Wearing appropriate protective gear during sports
- Avoiding direct trauma to the ear
- Proper management of underlying medical conditions
- Regular ear check-ups when recommended
Frequently Asked Questions
What are the common symptoms of hemotympanum and how can I identify it? Hemotympanum typically presents with hearing loss, ear fullness, and possible discomfort. The eardrum may appear dark or bluish when examined by a healthcare provider. Only a medical professional can make a definitive diagnosis.
What causes hemotympanum and which factors increase the risk of developing it? Hemotympanum can be caused by head trauma, barotrauma, skull fractures, blood disorders, or chronic ear conditions. Risk factors include participation in contact sports, blood disorders, and certain medical conditions affecting the ear.
How is hemotympanum diagnosed by healthcare professionals? Healthcare providers diagnose hemotympanum through otoscopic examination, physical assessment, medical history review, and sometimes imaging studies. They may also perform hearing tests to evaluate the impact on hearing function.
What treatment options are available for hemotympanum and when is medical intervention necessary? Treatment depends on the underlying cause and may range from watchful waiting to medical interventions. Immediate medical attention is necessary if hemotympanum results from trauma or is accompanied by severe symptoms.
Can hemotympanum lead to long-term hearing loss or other complications? Yes, untreated hemotympanum can potentially lead to long-term hearing loss, chronic ear problems, and tympanic membrane damage. Early diagnosis and appropriate treatment are essential to prevent these complications.