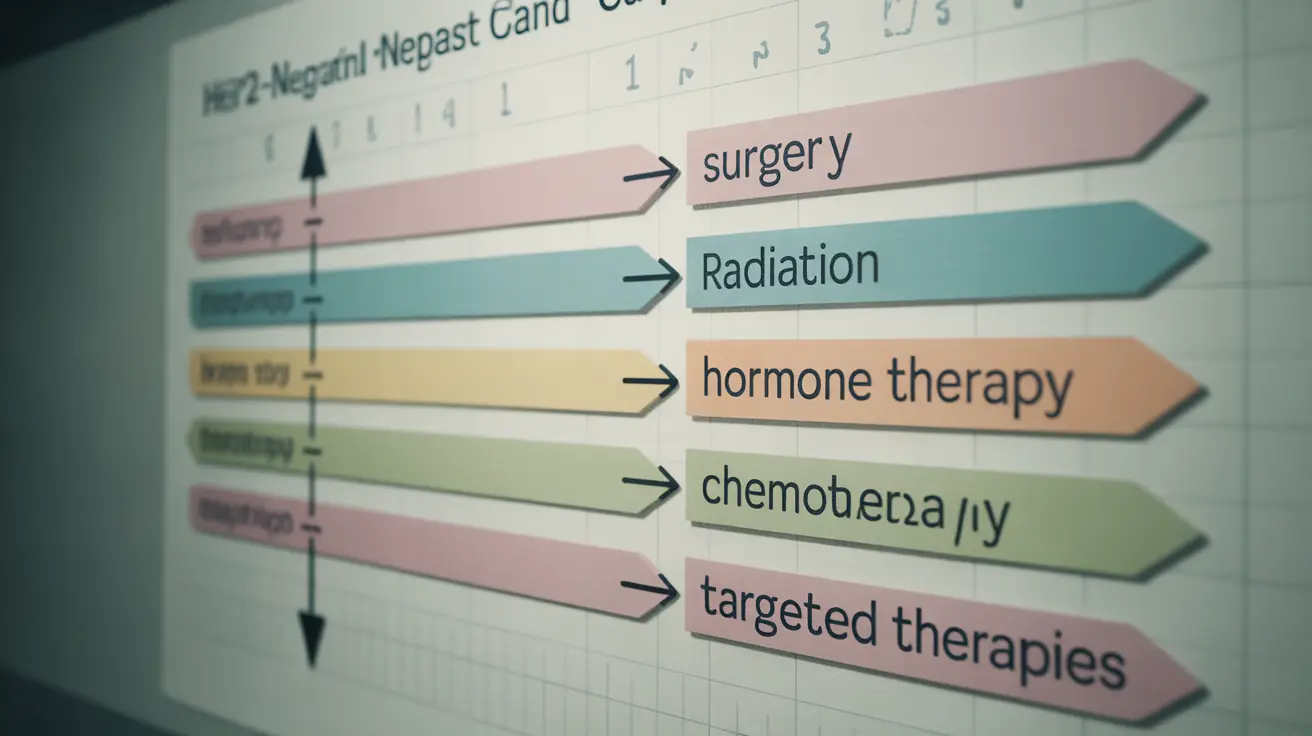
When diagnosed with HER2-negative breast cancer, understanding the available treatment options is crucial for making informed decisions about your care. This type of breast cancer lacks the human epidermal growth factor receptor 2 protein, which influences treatment approaches and outcomes. Modern medicine offers several effective strategies for managing HER2-negative breast cancer, with treatment plans typically tailored to each patient's specific situation.
Understanding HER2-Negative Breast Cancer
HER2-negative breast cancer is characterized by cancer cells that don't have high levels of the HER2 protein on their surface. This classification helps doctors determine the most effective treatment approach, as these cancers won't respond to HER2-targeted therapies but may be sensitive to other treatment methods.
Primary Treatment Approaches
Surgery Options
Surgery often serves as the primary treatment for HER2-negative breast cancer. Options typically include:
- Lumpectomy (breast-conserving surgery)
- Mastectomy (removal of the entire breast)
- Lymph node removal when necessary
Radiation Therapy
Radiation therapy frequently follows surgery, particularly after lumpectomy. This treatment helps eliminate any remaining cancer cells and reduces the risk of recurrence in the affected area.
Hormone Therapy for Hormone Receptor-Positive Cases
For HER2-negative breast cancers that are hormone receptor-positive, hormone therapy plays a crucial role in treatment. Common approaches include:
- Tamoxifen for pre- and postmenopausal women
- Aromatase inhibitors for postmenopausal women
- Ovarian suppression for premenopausal women
Chemotherapy Protocols
Chemotherapy may be recommended in several situations:
- Before surgery (neoadjuvant therapy)
- After surgery (adjuvant therapy)
- For advanced or metastatic disease
- When tumors are larger or have spread to lymph nodes
Advanced Treatment Options
Targeted Therapies
Modern targeted therapies have revolutionized HER2-negative breast cancer treatment:
- CDK4/6 inhibitors for hormone receptor-positive cases
- PARP inhibitors for patients with BRCA mutations
- PI3K inhibitors for specific molecular subtypes
Managing Metastatic Disease
Treatment for advanced HER2-negative breast cancer focuses on:
- Controlling disease progression
- Managing symptoms
- Maintaining quality of life
- Combining various treatment modalities as needed
Frequently Asked Questions
What are the main treatment options for HER2-negative breast cancer?
The main treatment options include surgery, radiation therapy, hormone therapy (for hormone receptor-positive cases), chemotherapy, and targeted therapies. Treatment plans are typically individualized based on cancer stage, hormone receptor status, and other patient-specific factors.
How is hormone therapy used to treat HER2-negative, hormone receptor-positive breast cancer?
Hormone therapy works by either blocking hormone receptors or reducing hormone production. Treatment options vary based on menopausal status and may include tamoxifen, aromatase inhibitors, or ovarian suppression methods. These treatments typically continue for 5-10 years.
When is chemotherapy recommended for HER2-negative breast cancer patients?
Chemotherapy is typically recommended for larger tumors, lymph node involvement, high-grade cancers, or triple-negative breast cancer. It may be given before surgery to shrink tumors or after surgery to reduce recurrence risk.
What role do targeted therapies like CDK4/6 inhibitors and PARP inhibitors play in HER2-negative breast cancer treatment?
CDK4/6 inhibitors are used in hormone receptor-positive, HER2-negative breast cancer to enhance hormone therapy effectiveness. PARP inhibitors target specific DNA repair defects in cancers with BRCA mutations, offering an additional treatment option for eligible patients.
How is advanced or metastatic HER2-negative breast cancer managed to improve quality of life?
Management of advanced HER2-negative breast cancer involves a combination of treatments to control disease progression and maintain quality of life. This may include systemic therapies, pain management, supportive care, and regular monitoring to adjust treatment as needed.