Understanding how heredity affects cholesterol levels is crucial for managing cardiovascular health. While genetics can play a role in cholesterol regulation, the relationship between heredity and cholesterol levels is more complex than many people realize. This article explores the various ways genetics influence cholesterol levels and what you can do to maintain healthy numbers, regardless of your family history.
Understanding Genetic Influence on Cholesterol
While heredity has some influence on cholesterol levels, it's important to note that for most people, lifestyle factors play a more significant role. The exception is a genetic condition called familial hypercholesterolemia (FH), which affects about 1 in 250 people and causes very high cholesterol levels from birth.
The Role of Genetics in Normal Cholesterol Regulation
For individuals without familial hypercholesterolemia, genetics typically accounts for only about 20-30% of total cholesterol variation. Environmental factors, diet, and physical activity levels often have a much stronger impact on cholesterol levels than genetic predisposition alone.
How Genes Affect Cholesterol Processing
Several genes influence how your body processes cholesterol, including:
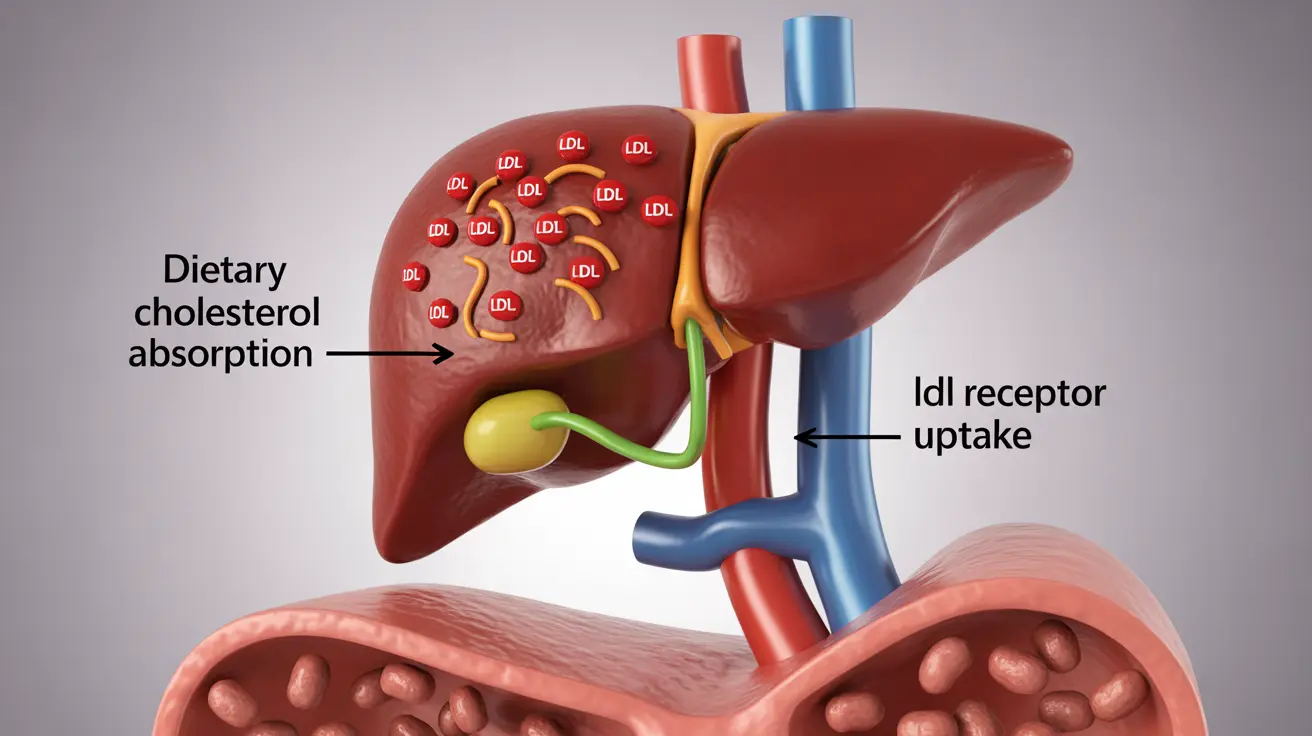
- LDL receptor genes that affect how cells remove cholesterol from blood
- Genes that regulate cholesterol production in the liver
- Genes involved in dietary cholesterol absorption
Familial Hypercholesterolemia: When Genetics Take Center Stage
Familial hypercholesterolemia is characterized by mutations that significantly impair the body's ability to remove LDL cholesterol from the blood. This condition requires early detection and aggressive treatment to prevent cardiovascular complications.
Gender Differences in FH
Research shows that men with FH typically develop cardiovascular disease about 10 years earlier than women with the condition. Women generally have some protection from hormones until menopause, after which their risk increases significantly.
Managing Cholesterol Through Lifestyle Changes
Even with a genetic predisposition to high cholesterol, lifestyle modifications can make a substantial difference. Key strategies include:
- Maintaining a heart-healthy diet low in saturated fats
- Regular physical activity
- Maintaining a healthy weight
- Avoiding tobacco use
- Limiting alcohol consumption
The Importance of Genetic Testing
Genetic testing can be valuable for individuals with very high cholesterol levels or a strong family history of early heart disease. This testing helps identify specific genetic variants and guides treatment decisions.
Frequently Asked Questions
How does genetics influence cholesterol levels in individuals without familial hypercholesterolemia?
Genetics typically accounts for 20-30% of cholesterol variation in people without FH. Most cholesterol levels are more significantly influenced by lifestyle factors and diet than by genetic factors alone.What are the symptoms and treatment options for familial hypercholesterolemia?
FH typically shows no physical symptoms but causes very high LDL cholesterol levels from birth. Treatment usually involves a combination of statins, other cholesterol-lowering medications, and strict lifestyle modifications.Can lifestyle changes significantly improve cholesterol levels in people with a family history of high cholesterol?
Yes, even with genetic predisposition, lifestyle changes can substantially impact cholesterol levels. Regular exercise, healthy diet, and weight management can often help maintain healthy cholesterol levels.How does familial hypercholesterolemia affect men and women differently in terms of heart disease risk?
Men with FH typically develop cardiovascular disease about a decade earlier than women. Women generally have some protection from estrogen until menopause, after which their cardiovascular risk increases significantly.What is the role of genetic testing in managing familial hypercholesterolemia, and who should consider it?
Genetic testing is recommended for individuals with very high cholesterol levels, especially those under 40, or those with a strong family history of early heart disease. The results help guide treatment strategies and identify family members who may need screening.