Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition that can cause significant concern for those affected and their loved ones. One of the most common questions people have about this condition is whether it can spread from person to person. Understanding the nature of HS is crucial for both patients and their families.
This comprehensive guide will explain the non-contagious nature of HS, its true causes, and how to effectively manage the condition. We'll also address common misconceptions and provide evidence-based information about this often misunderstood skin disorder.
The Non-Contagious Nature of Hidradenitis Suppurativa
Hidradenitis suppurativa is not contagious and cannot be transmitted from one person to another. This condition is an internal inflammatory process that develops due to complex factors within the body, rather than from external causes or infections. You cannot "catch" HS through physical contact, sharing personal items, or any other form of interaction with someone who has the condition.
Understanding the True Causes of HS
The development of hidradenitis suppurativa is linked to several internal factors:
- Genetic predisposition
- Hormonal changes
- Immune system dysfunction
- Follicular occlusion (blocked hair follicles)
- Inflammatory responses
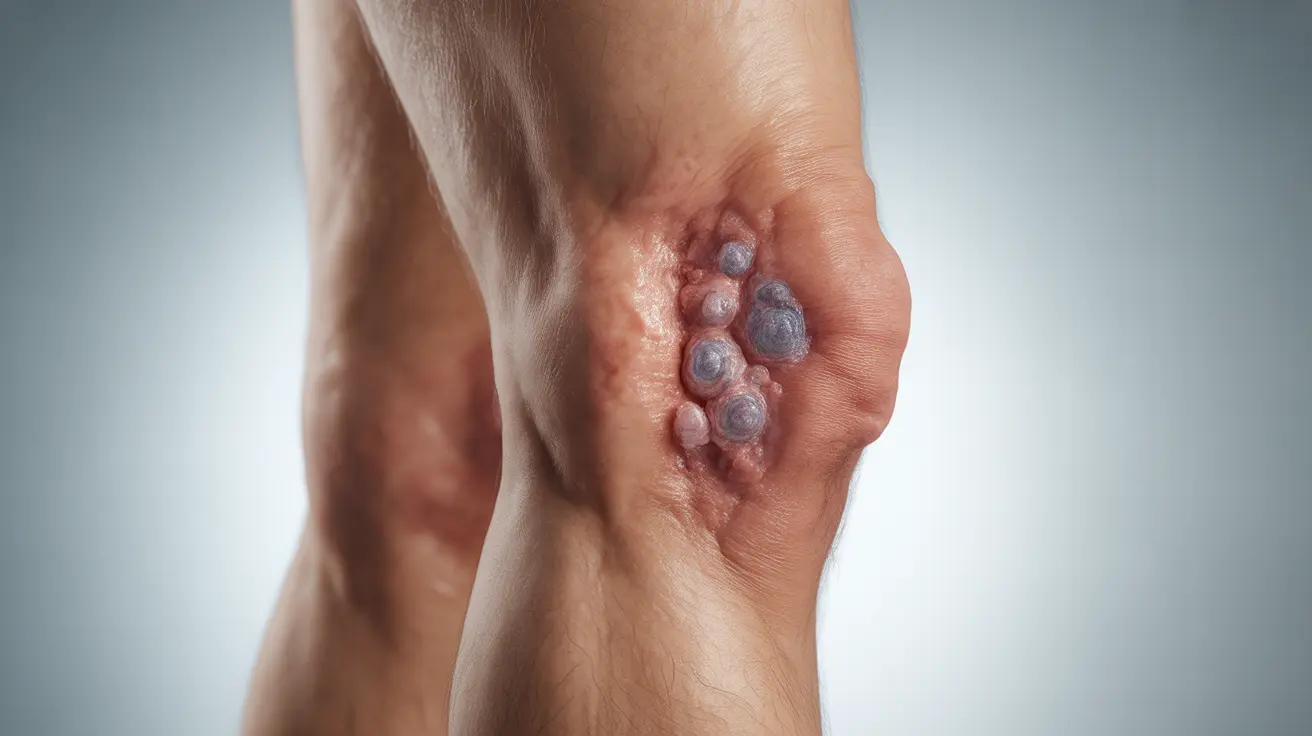
The condition occurs when hair follicles become blocked and inflamed, leading to painful bumps and abscesses in areas where skin rubs together, such as the armpits, groin, and under the breasts.
Common Misconceptions and Stigma
Many people mistakenly believe that HS is caused by poor hygiene or is infectious. This misconception can lead to unnecessary social isolation and emotional distress for those affected. It's important to understand that HS is a medical condition that requires proper medical attention and support, not social distancing or isolation.
Treatment and Management Options
While HS cannot be cured, several treatment options can help manage symptoms and prevent flare-ups:
- Topical and oral antibiotics
- Anti-inflammatory medications
- Biologics for severe cases
- Surgical interventions when necessary
- Wound care and dressing
Working with a dermatologist or healthcare provider is essential to develop an effective treatment plan tailored to individual needs and severity of symptoms.
Lifestyle Modifications for Better Management
Several lifestyle changes can help reduce the frequency and severity of HS flares:
- Maintaining a healthy weight
- Wearing loose-fitting, breathable clothing
- Avoiding smoking
- Managing stress levels
- Following proper skin care routines
- Avoiding triggers that may cause flares
Frequently Asked Questions
Is hidradenitis suppurativa contagious or can it be spread from person to person?
No, HS is not contagious and cannot be transmitted between people. It is an internal inflammatory condition that develops due to genetic and environmental factors within an individual's body.
What causes hidradenitis suppurativa if it is not due to infection or poor hygiene?
HS is caused by a combination of genetic predisposition, hormonal factors, immune system dysfunction, and follicular occlusion. Poor hygiene does not cause HS, although good hygiene practices can help manage symptoms.
How is hidradenitis suppurativa treated and what are the available management options?
Treatment options include topical and oral medications, biologics, surgical interventions, and lifestyle modifications. The appropriate treatment plan depends on the severity of the condition and individual patient factors.
Can hidradenitis suppurativa be mistaken for a sexually transmitted infection or acne?
Yes, HS can be mistaken for other skin conditions, including STIs or severe acne, due to similar appearance. However, HS has distinct characteristics and typically occurs in specific areas of the body. Professional medical evaluation is important for correct diagnosis.
What lifestyle changes can help reduce flare-ups or symptoms of hidradenitis suppurativa?
Key lifestyle changes include maintaining a healthy weight, quitting smoking, wearing loose-fitting clothes, practicing good wound care, managing stress, and identifying and avoiding personal triggers that may cause flares.