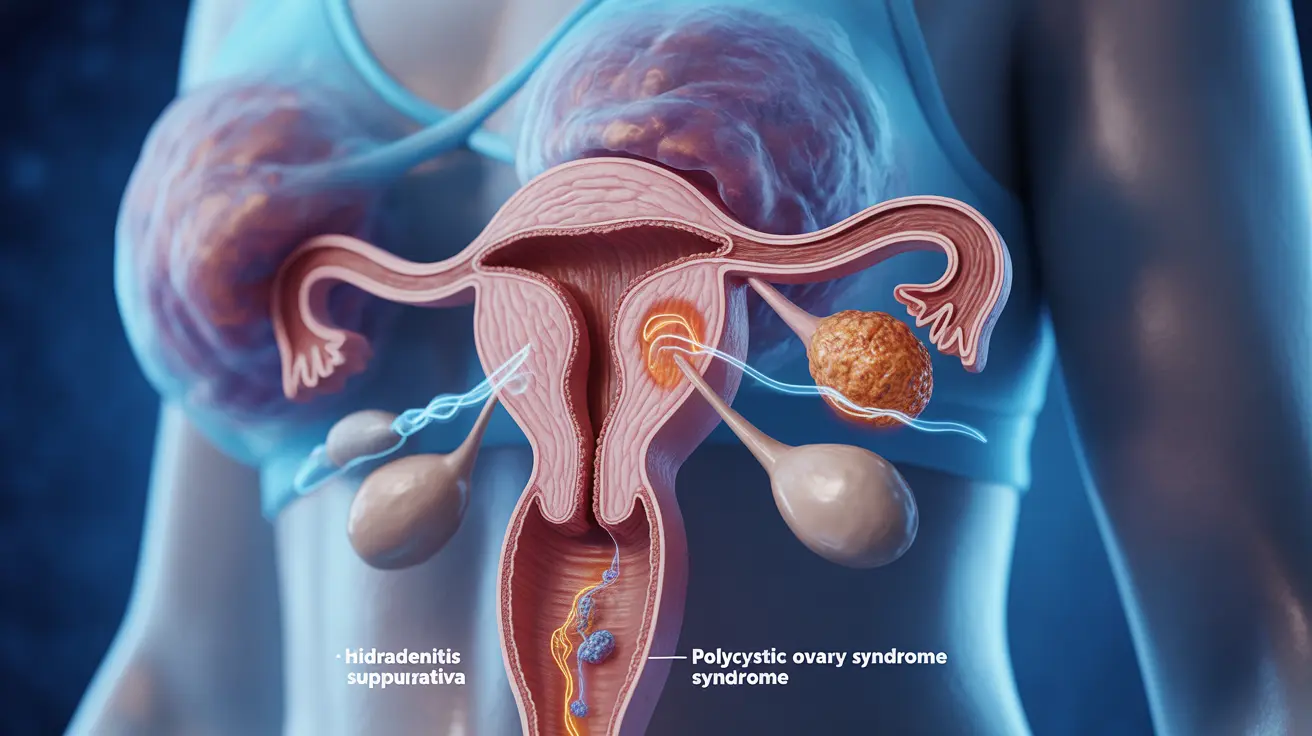
Living with either hidradenitis suppurativa (HS) or polycystic ovary syndrome (PCOS) can be challenging, but when these conditions occur together, they present unique challenges that require special attention. Research has shown a significant connection between these two conditions, with many patients experiencing symptoms of both simultaneously.
Understanding how these conditions interact and influence each other is crucial for proper management and treatment. This comprehensive guide explores the relationship between HS and PCOS, helping you recognize symptoms and discover effective management strategies.
The Link Between Hidradenitis Suppurativa and PCOS
Hidradenitis suppurativa and PCOS share several underlying factors that contribute to their connection. Both conditions are influenced by hormonal imbalances, inflammation, and metabolic factors. Research suggests that women with HS are more likely to develop PCOS, and vice versa, indicating a bidirectional relationship between these conditions.
Common Risk Factors
Several shared risk factors contribute to both conditions:
- Hormonal imbalances, particularly androgens
- Insulin resistance
- Obesity
- Chronic inflammation
- Genetic predisposition
Recognizing PCOS Symptoms When You Have HS
If you have hidradenitis suppurativa, being aware of potential PCOS symptoms is essential for early detection and treatment. Common PCOS indicators include:
- Irregular menstrual cycles
- Excessive hair growth (hirsutism)
- Acne
- Weight gain
- Hair loss or thinning
- Difficulty getting pregnant
The Role of Hormones
Hormonal imbalances play a crucial role in both conditions. Elevated androgen levels can trigger or worsen both HS and PCOS symptoms. Understanding this hormonal connection is vital for developing effective treatment strategies.
Impact on Disease Progression
Hormonal fluctuations can affect the severity and frequency of HS flares while simultaneously influencing PCOS symptoms. This interaction often requires a coordinated treatment approach that addresses both conditions.
Treatment Approaches
Managing both conditions typically requires a multi-faceted approach:
Medical Treatments
- Hormonal therapy
- Anti-inflammatory medications
- Topical treatments for HS
- Insulin-sensitizing medications
- Antibiotics when necessary
Surgical Options
In severe cases of HS, surgical intervention might be necessary, even while managing PCOS. Your healthcare provider can help determine the best timing and approach for any surgical procedures.
Lifestyle Management Strategies
Lifestyle modifications can significantly impact both conditions:
- Maintaining a healthy weight
- Following an anti-inflammatory diet
- Regular exercise
- Stress management
- Proper skincare routine
- Avoiding trigger foods
Frequently Asked Questions
What is the connection between hidradenitis suppurativa and polycystic ovary syndrome (PCOS)?
Hidradenitis suppurativa and PCOS share common underlying factors including hormonal imbalances, inflammation, and metabolic dysfunction. Both conditions often occur together and can influence each other's severity and progression.
What symptoms of PCOS should people with hidradenitis suppurativa watch for?
People with HS should watch for irregular menstrual cycles, excessive hair growth, acne, unexplained weight gain, hair loss, and fertility issues as potential signs of PCOS.
How do hormonal imbalances affect both hidradenitis suppurativa and PCOS?
Hormonal imbalances, particularly elevated androgens, can trigger or worsen symptoms of both conditions. These imbalances can lead to increased inflammation, skin changes, and metabolic disruptions affecting both HS and PCOS.
What treatments are available to manage hidradenitis suppurativa in people who also have PCOS?
Treatment options include hormonal therapy, anti-inflammatory medications, topical treatments, insulin-sensitizing drugs, and in some cases, surgery for HS. Treatment plans are typically customized to address both conditions simultaneously.
Can lifestyle changes help reduce symptoms of both hidradenitis suppurativa and PCOS?
Yes, lifestyle modifications such as maintaining a healthy weight, following an anti-inflammatory diet, regular exercise, and stress management can significantly improve symptoms of both conditions.