Hormonal headaches can significantly impact daily life, particularly for those experiencing them during menstrual cycles or hormonal changes. Understanding where these headaches typically occur and recognizing their patterns is crucial for proper diagnosis and treatment.
These distinctive headaches often follow specific patterns and locations, making them identifiable from other types of headaches. Learning to recognize their characteristics can help you better manage and treat them effectively.
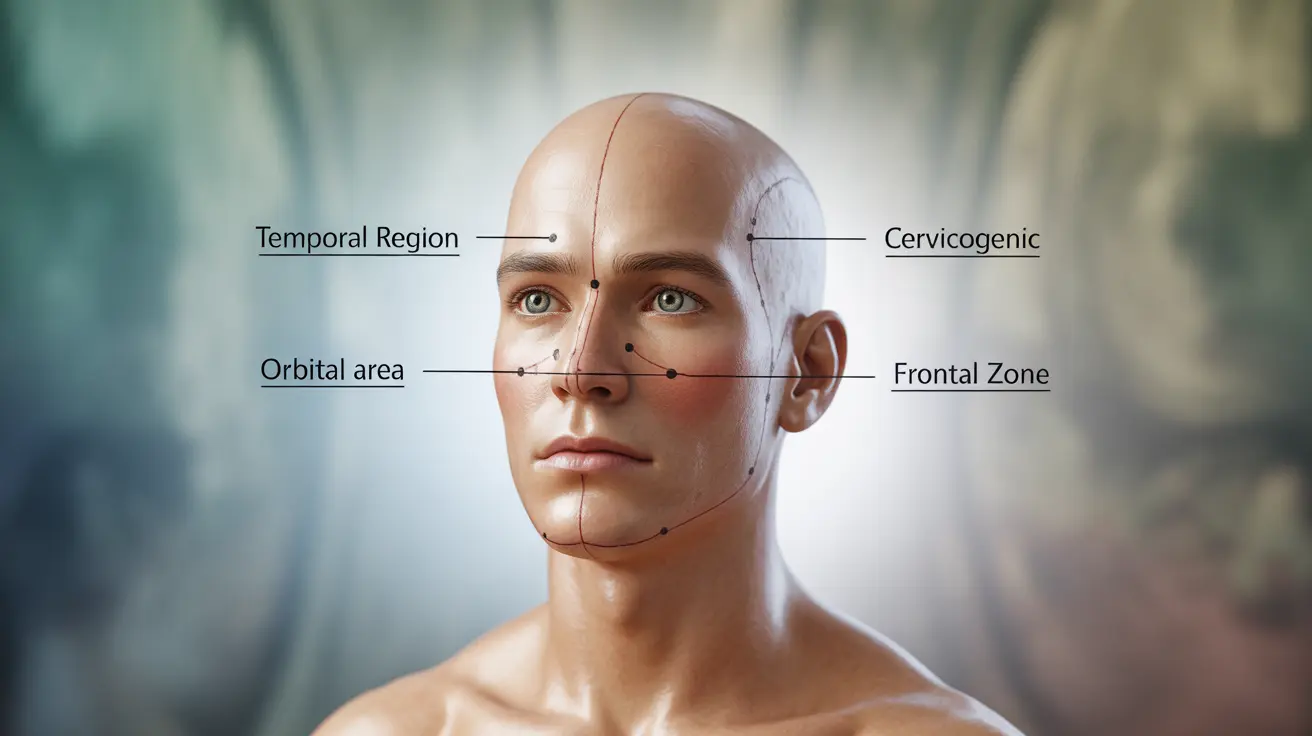
Common Locations of Hormonal Headaches
Hormonal headaches typically present in several characteristic locations:
- One side of the head (unilateral pain)
- Behind the eyes
- Temple area
- Base of the neck
- Across the forehead
The pain may shift from one side to another during the same episode or in subsequent headaches. Many people report that the pain tends to be more intense on one particular side.
Understanding the Hormone-Headache Connection
Hormonal headaches are closely linked to fluctuations in estrogen and progesterone levels. These changes most commonly occur during:
- Menstrual cycles
- Pregnancy
- Perimenopause and menopause
- Hormone replacement therapy
- Birth control use or discontinuation
The sudden drops in estrogen levels, particularly before menstruation, can trigger these headaches and influence their location and intensity.
Identifying Hormonal Headaches
Several key characteristics can help distinguish hormonal headaches from other types:
- Regular occurrence with menstrual cycles
- Predictable timing related to hormonal changes
- Duration typically lasting 4-72 hours
- Associated symptoms like nausea and light sensitivity
- Pattern of location consistency
Treatment Approaches
Medication Options
Several medication strategies can help manage hormonal headaches:
- Over-the-counter pain relievers
- Prescription migraine medications
- Hormonal treatments
- Preventive medications
Lifestyle Modifications
Implementing certain lifestyle changes can help reduce the frequency and severity of hormonal headaches:
- Regular sleep schedule
- Stress management techniques
- Consistent exercise routine
- Dietary modifications
- Proper hydration
Prevention Strategies
Taking proactive steps can help prevent or minimize hormonal headaches:
- Tracking headache patterns
- Identifying and avoiding triggers
- Maintaining hormonal balance through medical supervision
- Regular exercise and stress management
- Consistent sleep patterns
Frequently Asked Questions
Where on the head are hormonal headaches usually located?
Hormonal headaches typically occur on one side of the head, though they can affect both sides. Common locations include behind the eyes, in the temple area, at the base of the neck, or across the forehead. The pain location may shift during an episode.
What causes hormonal headaches to occur around the menstrual cycle?
Hormonal headaches during menstrual cycles are primarily triggered by drops in estrogen levels, particularly in the days leading up to menstruation. This hormonal fluctuation can affect blood vessels and pain receptors in the brain.
How can I tell if my headache is related to hormonal changes or something else?
Hormonal headaches typically follow a predictable pattern aligned with your menstrual cycle or other hormonal changes. They often occur at the same time each month, last between 4-72 hours, and may be accompanied by nausea, light sensitivity, and consistent pain locations.
What treatments are effective for managing hormonal or menstrual migraines?
Effective treatments include over-the-counter pain relievers, prescription migraine medications, hormonal treatments, and preventive medications. A combination of medical treatment and lifestyle modifications often provides the best results.
Can lifestyle changes help prevent or reduce the severity of hormonal headaches?
Yes, lifestyle changes can significantly impact hormonal headaches. Regular exercise, consistent sleep patterns, stress management, proper hydration, and dietary modifications can help reduce both the frequency and severity of these headaches.