For many expectant mothers, understanding the implications of multiple cesarean sections (C-sections) is crucial for family planning. While C-sections are generally safe procedures, each subsequent surgery presents unique considerations and potential risks that healthcare providers must carefully evaluate.
This comprehensive guide explores the factors that determine how many C-sections a person can safely undergo, the associated risks, and important considerations for future pregnancies.
Medical Considerations for Multiple C-Sections
Healthcare providers evaluate several key factors when determining the safety of multiple C-sections for individual patients. These factors include:
- Previous surgical healing
- Uterine wall thickness
- Overall health status
- Presence of adhesions
- Recovery time between pregnancies
Understanding Surgical Changes
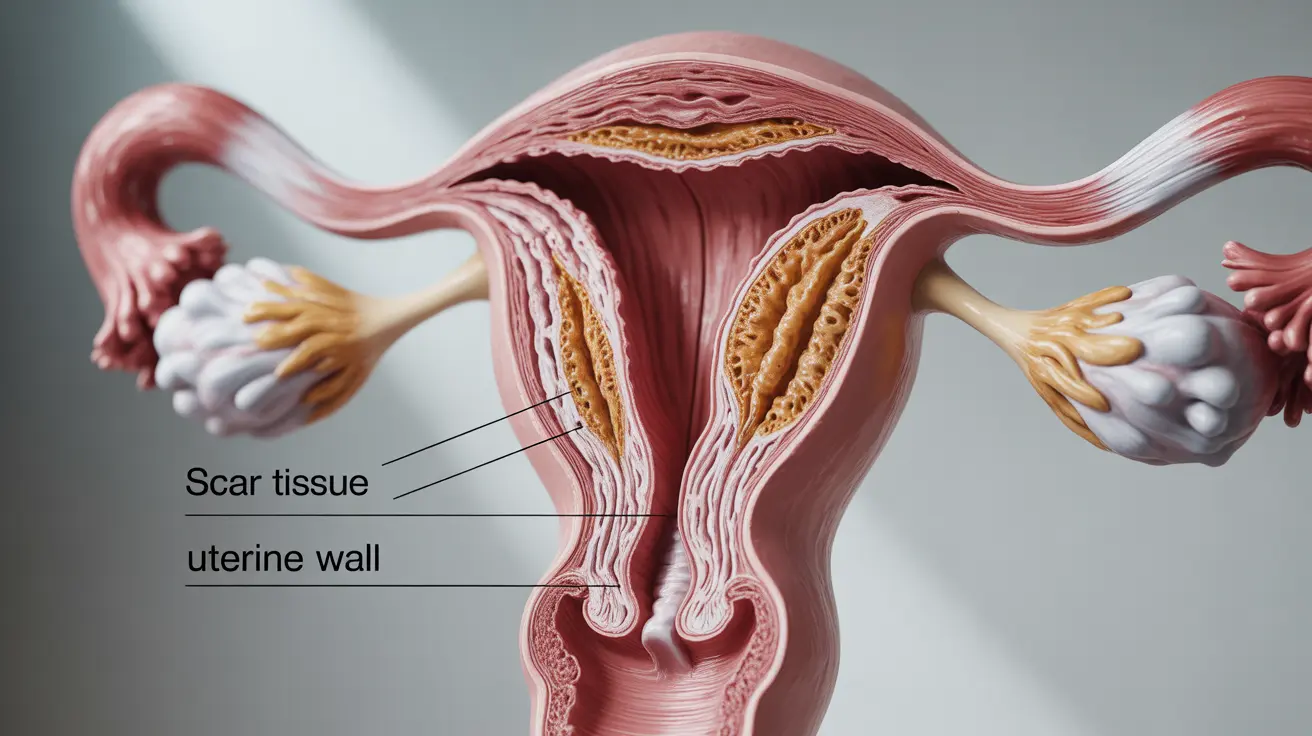
Each C-section creates scar tissue that can affect future pregnancies. The accumulation of scar tissue with each procedure can make subsequent surgeries more challenging and potentially increase risks. Medical professionals carefully monitor these changes through imaging and physical examinations.
Potential Risks and Complications
The risks associated with multiple C-sections typically increase with each subsequent procedure. Common complications may include:
- Bladder and bowel adhesions
- Increased bleeding during surgery
- Higher risk of placental problems
- Longer recovery periods
- Potential for uterine rupture
Managing Complications
Healthcare providers implement specific strategies to minimize risks during repeat C-sections, including careful surgical planning, enhanced monitoring, and specialized surgical techniques. These approaches help ensure the safest possible outcomes for both mother and baby.
Recovery and Timing Between Procedures
Proper healing time between C-sections is crucial for reducing complications. Most medical professionals recommend waiting at least 18-24 months between pregnancies to allow for optimal recovery and reduce risks in subsequent procedures.
Planning Future Pregnancies
When considering future pregnancies after multiple C-sections, healthcare providers evaluate several factors:
- Previous surgical outcomes
- Current health status
- Quality of uterine healing
- Individual risk factors
- Personal family planning goals
Frequently Asked Questions
What are the general risks associated with having multiple C-sections, and how do they impact future pregnancies?
Multiple C-sections can increase risks such as surgical adhesions, bleeding complications, and placental issues in future pregnancies. Each subsequent C-section typically carries higher risks than the previous one, particularly regarding surgical complexity and healing time.
How do healthcare providers determine the safe number of C-sections for an individual, and what factors are considered?
Healthcare providers evaluate factors including previous surgical outcomes, uterine wall integrity, overall health status, and healing between pregnancies. They also consider individual risk factors and medical history to determine safety for additional procedures.
What are the potential complications of having more than two C-sections, and how can they be managed?
Complications after multiple C-sections may include increased adhesions, bleeding risks, and placental abnormalities. These are managed through careful surgical planning, enhanced monitoring, and specialized surgical techniques tailored to each patient's situation.
Is it safe to plan a vaginal delivery after having multiple C-sections, and what are the deciding factors?
Vaginal birth after multiple C-sections (VBAC) is generally not recommended due to increased risks of uterine rupture. Key factors in this decision include the number of previous C-sections, type of uterine incision, and overall health status.
How long should a woman wait between C-sections to ensure optimal recovery and minimize risks in future pregnancies?
Medical professionals typically recommend waiting 18-24 months between C-sections to allow for complete healing and reduce risks in subsequent pregnancies. This timeframe helps ensure optimal uterine recovery and reduces complications in future procedures.