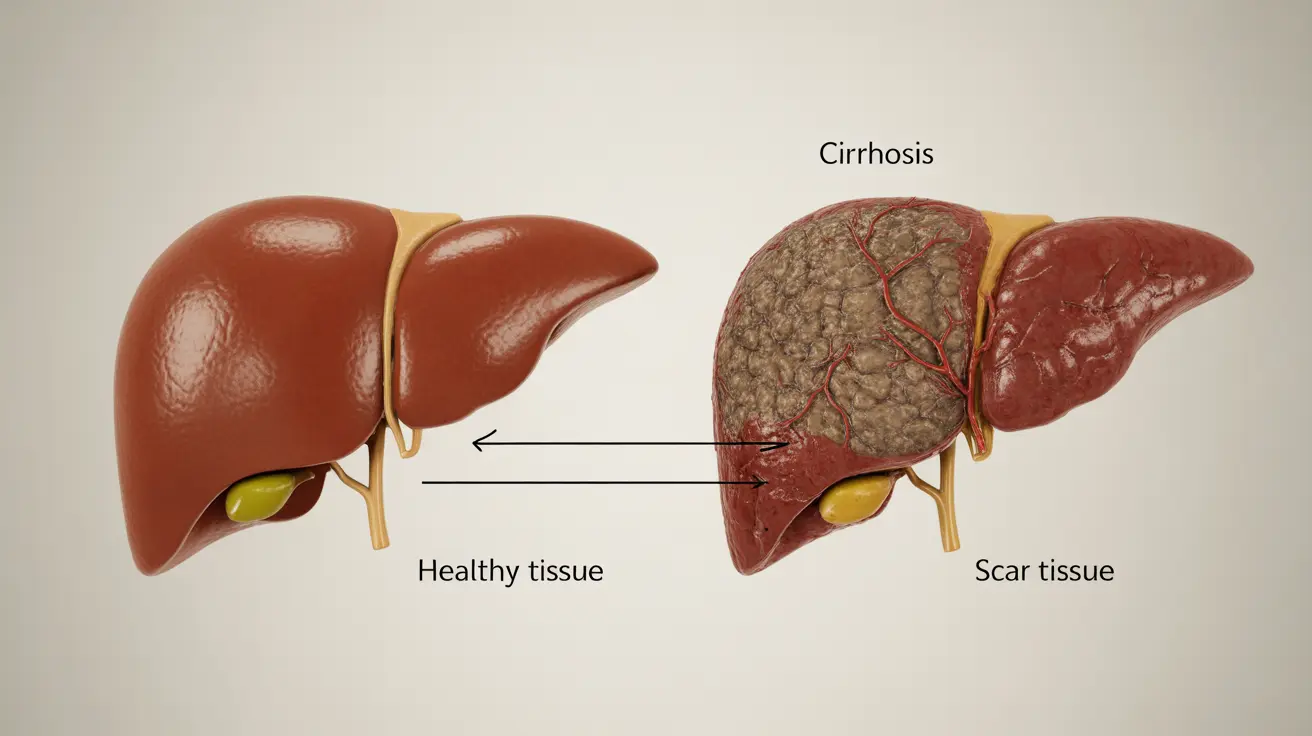
Alcohol-related liver cirrhosis is a serious medical condition that develops when prolonged alcohol consumption causes permanent scarring of the liver tissue. Understanding how much alcohol it takes to develop cirrhosis is crucial for anyone who drinks regularly, as this knowledge can help prevent irreversible liver damage.
While individual tolerance and susceptibility to liver damage vary significantly, certain patterns of alcohol consumption put people at higher risk for developing cirrhosis. This article explores the relationship between alcohol consumption and liver cirrhosis, including risk factors, early warning signs, and prevention strategies.
The Alcohol-Cirrhosis Connection: Understanding the Risks
The development of cirrhosis depends on several factors, including:
- Duration of alcohol use
- Daily amount consumed
- Individual genetic factors
- Gender differences in alcohol metabolism
- Overall health status
- Presence of other liver conditions
Research indicates that consuming more than 30 grams of alcohol (about 2-3 standard drinks) daily for 10 years or longer significantly increases the risk of developing cirrhosis. However, some individuals may develop liver problems with less alcohol consumption, while others might appear resistant to liver damage despite heavy drinking.
Gender Differences in Alcohol-Related Liver Disease
Women face a higher risk of developing alcohol-related liver disease compared to men, even when consuming smaller amounts of alcohol. This increased vulnerability is due to several factors:
- Higher blood alcohol concentrations from the same amount of alcohol
- Lower levels of alcohol-metabolizing enzymes
- Hormonal differences affecting liver function
- Generally smaller body mass and different body composition
Early Warning Signs of Alcohol-Related Liver Disease
Recognizing early symptoms is crucial for preventing progression to cirrhosis. Common early signs include:
- Fatigue and weakness
- Loss of appetite
- Nausea and vomiting
- Abdominal pain or tenderness
- Yellowing of the skin and eyes (jaundice)
- Spider-like blood vessels on the skin
- Unexplained weight loss
Treatment and Recovery Options
The most crucial step in treating alcohol-related cirrhosis is complete alcohol cessation. Additional treatment approaches may include:
- Medical supervision and support during alcohol withdrawal
- Nutritional therapy and dietary modifications
- Medications to manage complications
- Regular monitoring of liver function
- Treatment of related health issues
Prevention and Lifestyle Changes
Several lifestyle modifications can help prevent or slow the progression of alcohol-related liver disease:
- Limiting or avoiding alcohol consumption
- Maintaining a balanced, healthy diet
- Regular exercise and weight management
- Avoiding medications that can stress the liver
- Regular medical check-ups and liver function tests
Frequently Asked Questions
How much alcohol does it take to cause liver cirrhosis?
Consuming more than 2-3 standard drinks daily for 10 or more years significantly increases cirrhosis risk. However, the exact amount varies by individual, with some developing problems with less consumption and others showing more resistance.
Can drinking small amounts of alcohol still lead to cirrhosis, especially in women?
Yes, women are more susceptible to alcohol-related liver damage and may develop cirrhosis with lower amounts of alcohol consumption due to biological differences in how their bodies process alcohol.
What are the early symptoms of alcohol-related liver cirrhosis to watch for?
Early warning signs include fatigue, loss of appetite, nausea, abdominal pain, jaundice, and the appearance of spider-like blood vessels on the skin. These symptoms should prompt immediate medical attention.
How is alcohol-related liver cirrhosis treated and can the liver heal after stopping alcohol?
Treatment primarily involves complete alcohol cessation. While the liver cannot fully recover from cirrhosis, stopping alcohol use can prevent further damage and allow for some healing. Treatment may include medical supervision, nutritional support, and medications to manage complications.
What lifestyle changes can help prevent or slow the progression of alcohol-related cirrhosis?
Key lifestyle changes include abstaining from alcohol, maintaining a healthy diet, exercising regularly, avoiding harmful medications, and getting regular medical check-ups. These changes, especially when implemented early, can significantly impact liver health.