The relationship between hypoglycemia and anorexia is a critical medical concern that requires careful attention and understanding. When someone with anorexia experiences hypoglycemia, or low blood sugar, it can lead to serious health complications and requires immediate medical intervention.
This comprehensive guide explores how anorexia affects blood sugar levels, the associated risks, and essential management strategies during recovery. Understanding these connections is crucial for both patients and healthcare providers in preventing and treating hypoglycemic episodes.
The Connection Between Anorexia and Hypoglycemia
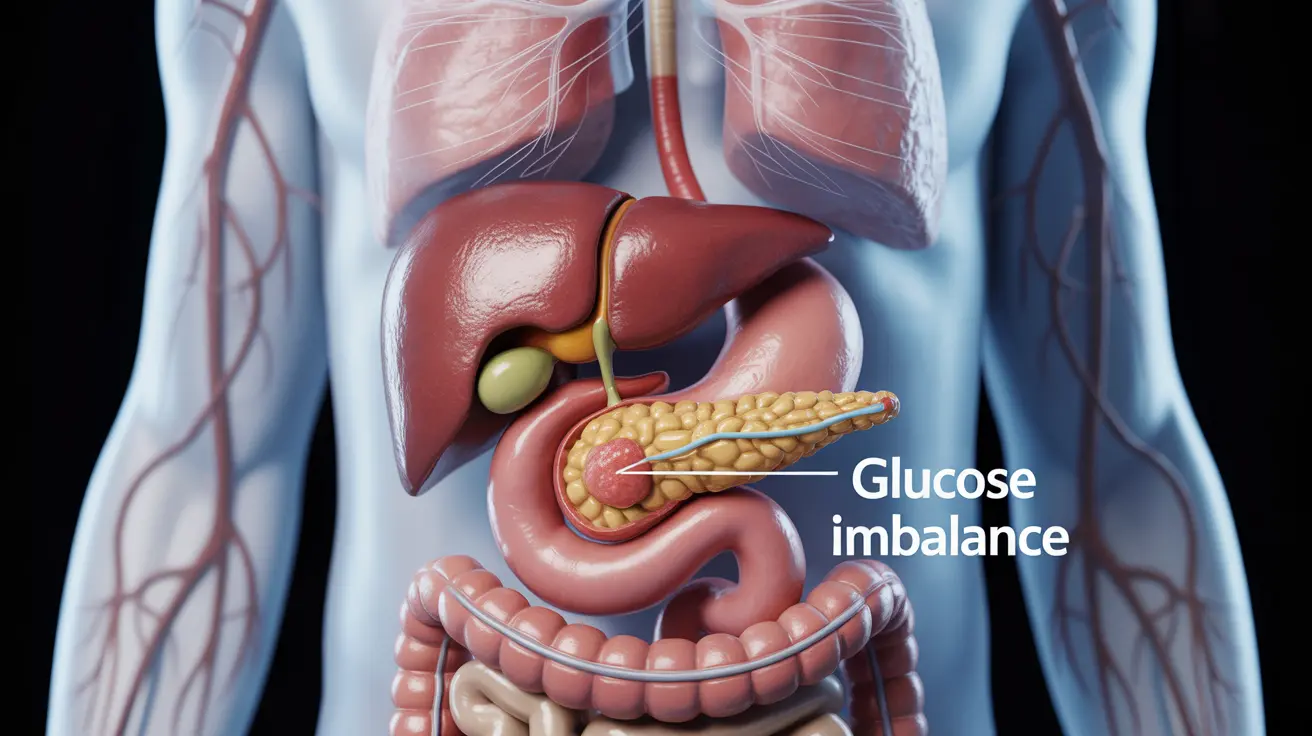
Anorexia nervosa can significantly impact the body's ability to maintain stable blood sugar levels. When the body is deprived of adequate nutrition, it struggles to regulate glucose effectively, leading to dangerous drops in blood sugar levels. This metabolic disruption occurs because the body lacks the necessary nutrients and calories to maintain proper glucose homeostasis.
Key Mechanisms Behind Blood Sugar Disruption
- Depleted glycogen stores due to insufficient caloric intake
- Impaired gluconeogenesis from lack of protein intake
- Hormonal imbalances affecting insulin and glucose regulation
- Compromised liver function due to malnutrition
Recognizing Hypoglycemic Symptoms in Anorexia
- Shakiness and trembling
- Excessive sweating
- Confusion and difficulty concentrating
- Weakness and fatigue
- Rapid heartbeat
- Anxiety and irritability
- In severe cases, loss of consciousness
The Refeeding Challenge
During anorexia recovery, refeeding must be carefully managed to prevent refeeding syndrome, which can worsen hypoglycemia. Healthcare providers typically implement a structured refeeding protocol that gradually increases caloric intake while monitoring blood sugar levels closely.
Safe Refeeding Practices
- Regular blood glucose monitoring
- Balanced nutrient introduction
- Electrolyte supplementation
- Medical supervision
- Gradual caloric increase
Prevention and Management Strategies
- Regular meal scheduling
- Balanced nutrition planning
- Continuous blood sugar monitoring
- Professional medical oversight
- Emergency glucose source availability
Treatment Approaches
- Quick-acting glucose sources for emergency situations
- Structured meal plans
- Regular medical check-ups
- Psychological support
- Nutritional counseling
Frequently Asked Questions
- What are the common symptoms of hypoglycemia caused by severe anorexia or malnutrition?
Common symptoms include shakiness, sweating, confusion, weakness, rapid heartbeat, and anxiety. In severe cases, individuals may experience loss of consciousness. These symptoms occur when blood sugar levels drop too low due to inadequate nutrition and disrupted metabolic processes.
- How does refeeding during anorexia recovery trigger hypoglycemia, and how can it be managed safely?
Refeeding can trigger hypoglycemia due to sudden changes in insulin production and glucose metabolism. Safe management involves carefully controlled caloric increases, regular blood sugar monitoring, and medical supervision to prevent refeeding syndrome and maintain stable blood glucose levels.
- What are the risks and potential complications of hypoglycemia in people with anorexia nervosa?
Risks include cognitive impairment, seizures, organ damage, cardiac complications, and in severe cases, coma. Long-term complications can affect multiple body systems and may lead to permanent damage if left untreated.
- How can hypoglycemia be prevented or monitored in individuals with severe anorexia during nutritional rehabilitation?
Prevention involves regular blood glucose monitoring, structured meal planning, and careful medical oversight. Healthcare providers should implement a comprehensive monitoring protocol that includes frequent blood tests, vital sign checks, and adjustment of nutrition plans as needed.
- What treatments are recommended for hypoglycemia related to anorexia, especially during episodes of low blood sugar?
Immediate treatment includes administering fast-acting glucose sources. Long-term treatment involves establishing regular eating patterns, nutritional counseling, medical monitoring, and addressing underlying psychological factors through therapy and support services.