The relationship between hypoglycemia (low blood sugar) and hypothyroidism (underactive thyroid) is complex and significant for those managing either or both conditions. Understanding how these conditions interact is crucial for proper diagnosis and treatment, as thyroid function plays a vital role in blood sugar regulation.
This comprehensive guide explores the connection between these conditions, helping you recognize important symptoms and understand proper management strategies.
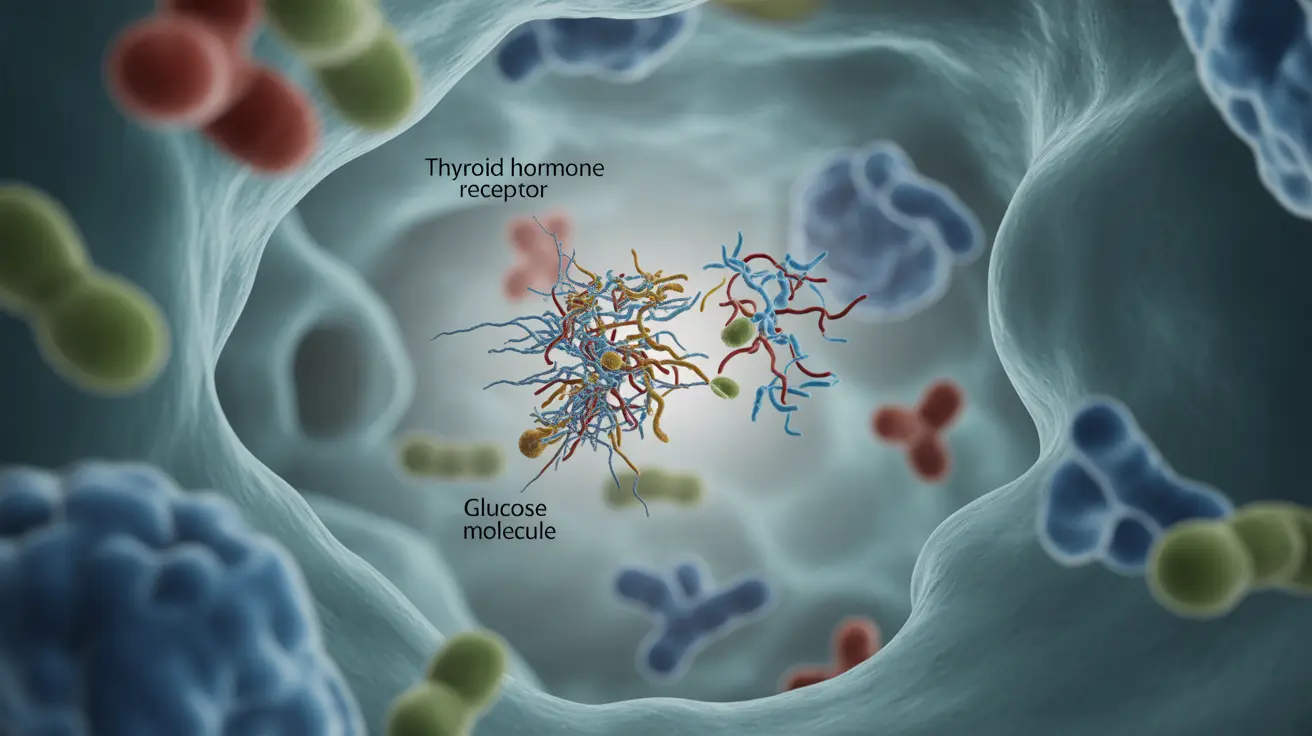
The Link Between Thyroid Function and Blood Sugar
Thyroid hormones play a crucial role in regulating metabolism and how your body processes glucose. When thyroid function is low (hypothyroidism), it can affect various aspects of blood sugar control:
- Slower metabolism of glucose
- Reduced insulin sensitivity
- Decreased gluconeogenesis (production of glucose in the liver)
- Altered absorption of medications that control blood sugar
Common Symptoms When Both Conditions Coexist
People experiencing both hypoglycemia and hypothyroidism may notice overlapping symptoms that can make diagnosis challenging:
- Fatigue and weakness
- Difficulty concentrating
- Anxiety or nervousness
- Sweating
- Irregular heartbeat
- Cold intolerance
- Weight changes
Impact on Diabetes Management
For individuals with diabetes, having hypothyroidism can make blood sugar control more challenging. The condition can affect:
- Insulin sensitivity
- Medication effectiveness
- Blood sugar monitoring accuracy
- Risk of severe hypoglycemic episodes
Treatment Considerations
Managing both conditions requires a careful, coordinated approach:
- Regular monitoring of thyroid levels
- Frequent blood sugar checks
- Proper timing of medications
- Dietary adjustments
- Regular communication with healthcare providers
Prevention and Management Strategies
Several strategies can help manage both conditions effectively:
- Keep a detailed symptom diary
- Monitor blood sugar levels regularly
- Take thyroid medication as prescribed
- Maintain consistent meal timing
- Carry quick-acting glucose sources
- Schedule regular medical check-ups
Frequently Asked Questions
How does hypothyroidism increase the risk of hypoglycemia? Hypothyroidism can increase hypoglycemia risk by slowing metabolism, reducing insulin clearance, and affecting how the body produces and processes glucose. This can lead to unexpected drops in blood sugar levels, especially in people taking diabetes medications.
What symptoms should I watch for that indicate hypoglycemia caused by hypothyroidism? Key symptoms include unusual fatigue, confusion, trembling, sweating, anxiety, and difficulty concentrating. These symptoms may be more pronounced when both conditions are present, and they might occur more frequently or be more severe than usual hypoglycemic episodes.
Can hypothyroidism affect blood sugar control if I have diabetes? Yes, hypothyroidism can significantly impact blood sugar control in diabetics by altering insulin sensitivity and affecting how the body processes glucose. This may require adjustments to diabetes medication dosages and more frequent blood sugar monitoring.
How is hypoglycemia managed in people who also have hypothyroidism? Management typically involves optimizing thyroid hormone replacement, careful blood sugar monitoring, appropriate timing of medications, and maintaining consistent meal schedules. Healthcare providers may need to adjust both thyroid and diabetes medications to achieve optimal control.
Should thyroid function be tested if I experience frequent low blood sugar episodes? Yes, thyroid function testing is recommended for people experiencing unexplained or frequent hypoglycemic episodes, as undiagnosed hypothyroidism could be a contributing factor. Regular thyroid monitoring can help ensure proper treatment and reduce the risk of complications.