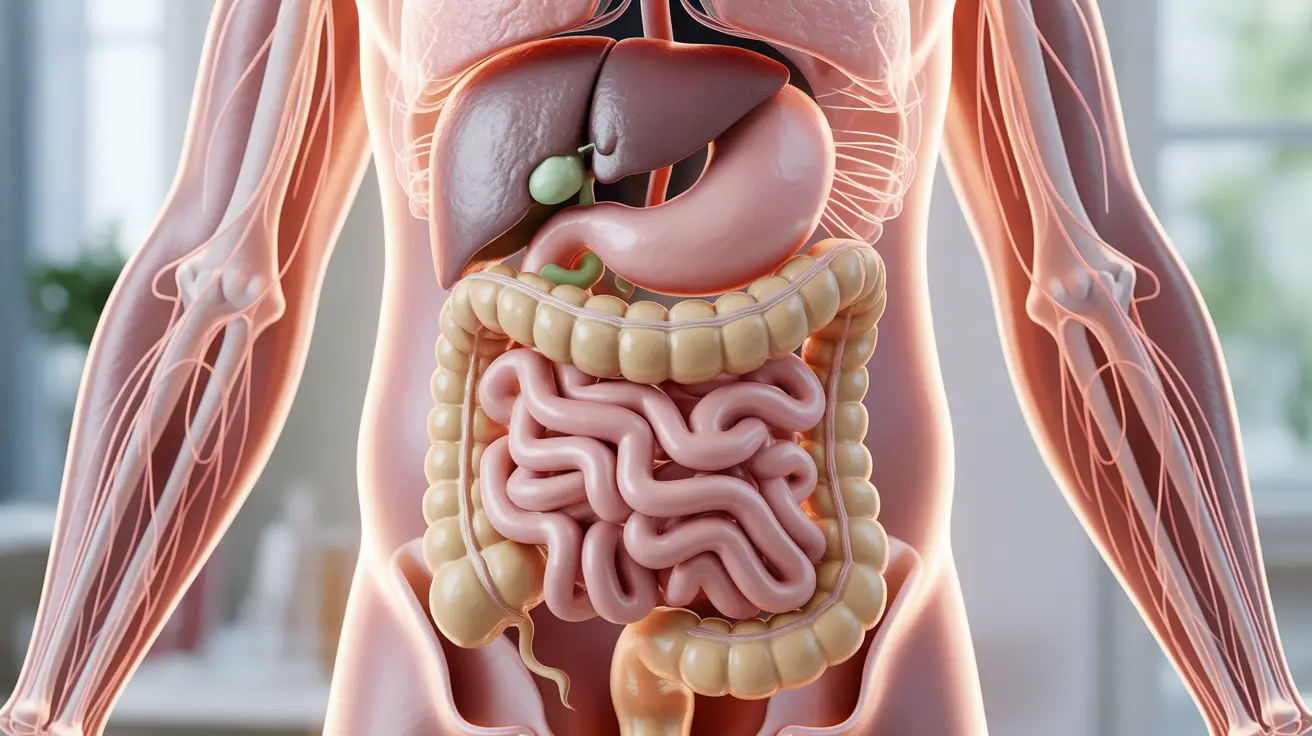
Living with Irritable Bowel Syndrome (IBS) can involve managing multiple digestive symptoms, and nausea is a significant concern for many patients. While IBS is primarily known for causing abdominal pain, bloating, and altered bowel habits, the relationship between IBS and nausea deserves careful attention.
Understanding how IBS can cause nausea and learning effective management strategies is crucial for improving quality of life for those affected by this chronic condition. Let's explore the connection between IBS and nausea, along with practical solutions for finding relief.
The Link Between IBS and Nausea
IBS can cause nausea through several mechanisms, including altered gut motility, heightened sensitivity to digestive processes, and the brain-gut connection. Many people with IBS experience nausea as part of their symptom complex, particularly during flare-ups of their condition.
The intensity and frequency of nausea can vary significantly among individuals, with some experiencing mild, occasional queasiness while others face more persistent symptoms that significantly impact their daily activities.
Common Triggers and Related Symptoms
Several factors can trigger or worsen nausea in people with IBS:
- Certain foods and dietary triggers
- Stress and anxiety
- Hormonal changes
- Medication side effects
- Irregular eating patterns
These triggers often work in conjunction with other IBS symptoms, creating a complex pattern of digestive disturbances that can be challenging to manage.
Managing Nausea Through Diet
Dietary modifications play a crucial role in managing IBS-related nausea. Consider these evidence-based strategies:
- Eating smaller, more frequent meals
- Avoiding trigger foods
- Staying well-hydrated
- Following a low-FODMAP diet under medical guidance
- Incorporating ginger or peppermint into your diet
Treatment Approaches
Several treatment options are available for managing nausea associated with IBS:
Medical Interventions
Healthcare providers may recommend:
- Anti-nausea medications
- IBS-specific medications
- Antispasmodics
- Antidepressants in some cases
Lifestyle Modifications
Complementary approaches can include:
- Stress management techniques
- Regular exercise
- Adequate sleep
- Mindfulness practices
- Acupuncture or other alternative therapies
When to Seek Medical Care
While some degree of nausea is common with IBS, certain situations warrant immediate medical attention:
- Severe or persistent nausea
- Vomiting that won't stop
- Significant weight loss
- Signs of dehydration
- New or changing symptoms
Frequently Asked Questions
Can irritable bowel syndrome (IBS) cause nausea and how common is it?
Yes, IBS can cause nausea, and studies suggest that approximately 30-40% of IBS patients experience nausea as part of their symptom complex. The frequency and severity can vary significantly among individuals.What triggers nausea in people with IBS and how is it related to other symptoms?
Nausea in IBS can be triggered by specific foods, stress, hormonal changes, and irregular eating patterns. It often occurs alongside other IBS symptoms like abdominal pain, bloating, and altered bowel movements, creating a interconnected pattern of digestive disturbances.How can dietary changes help manage nausea associated with IBS?
Dietary modifications such as eating smaller meals, identifying and avoiding trigger foods, following a low-FODMAP diet, and maintaining proper hydration can significantly help manage IBS-related nausea. Working with a registered dietitian can help develop an personalized eating plan.What treatments are available for nausea caused by IBS or its medications?
Treatment options include anti-nausea medications, IBS-specific drugs, dietary modifications, stress management techniques, and lifestyle changes. Some patients also benefit from complementary therapies like acupuncture or mindfulness practices.When should someone with IBS and nausea seek medical advice?
Seek immediate medical attention if you experience severe or persistent nausea, uncontrollable vomiting, significant weight loss, signs of dehydration, or if your symptoms significantly change or worsen. New or unusual symptoms should always be evaluated by a healthcare provider.