Immunophenotypic abnormalities play a crucial role in diagnosing and monitoring blood cancers like leukemia and lymphoma. These cellular markers help doctors identify cancer cells and determine the most effective treatment approaches. Understanding these abnormalities is essential for both healthcare providers and patients in managing blood cancer diagnoses and treatment plans.
This comprehensive guide explores how immunophenotypic abnormalities are detected, what they mean for diagnosis and treatment, and how they impact patient care throughout the cancer journey.
What Are Immunophenotypic Abnormalities?
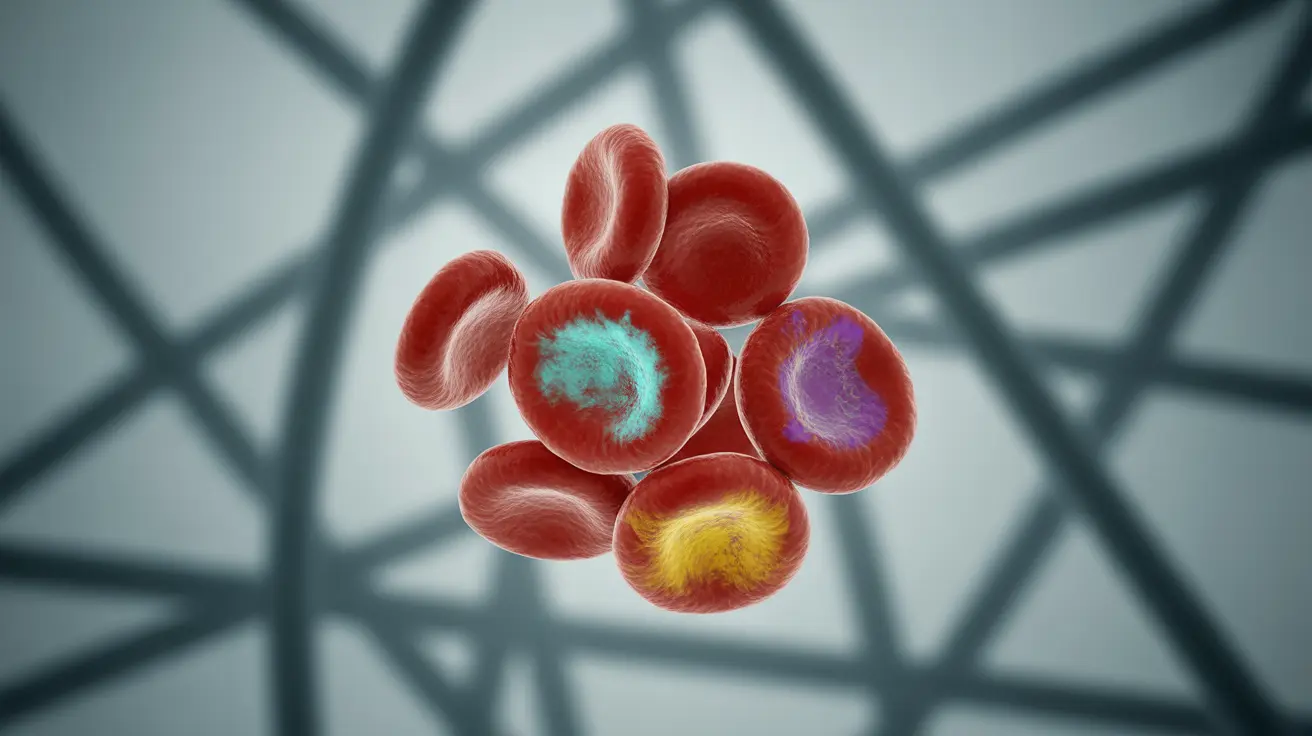
Immunophenotypic abnormalities are distinctive patterns of proteins and markers present on the surface of blood cells that differ from normal, healthy cells. These abnormal patterns serve as cellular "fingerprints" that help doctors identify and characterize different types of blood cancers.
These abnormalities can indicate:
- Unusual protein expressions on cell surfaces
- Missing or altered cellular markers
- Irregular combinations of normal markers
- Changes in the density of specific proteins
Detection Methods and Testing Process
Flow Cytometry Analysis
Flow cytometry is the primary method used to detect immunophenotypic abnormalities. This sophisticated technique allows scientists to analyze thousands of cells per second, identifying specific markers and protein patterns that indicate cancerous changes.
The process involves:
- Collecting blood or tissue samples
- Labeling cells with fluorescent markers
- Analyzing cells individually through laser detection
- Creating detailed profiles of cellular characteristics
Sample Collection and Preparation
Various types of samples can be used for immunophenotyping, including:
- Peripheral blood
- Bone marrow aspirates
- Lymph node tissue
- Other affected tissue samples
Clinical Significance and Applications
Understanding immunophenotypic abnormalities helps healthcare providers in several ways:
- Determining the specific type and subtype of blood cancer
- Monitoring treatment effectiveness
- Detecting minimal residual disease
- Predicting potential treatment outcomes
- Adjusting treatment strategies as needed
Impact on Treatment Planning
The pattern of immunophenotypic abnormalities can significantly influence treatment decisions by helping doctors:
- Select the most appropriate targeted therapies
- Determine optimal treatment timing
- Identify potential resistance to specific treatments
- Monitor treatment response effectively
Monitoring and Follow-up
Regular monitoring of immunophenotypic abnormalities throughout treatment helps healthcare providers:
- Track treatment effectiveness
- Detect early signs of disease progression
- Identify potential relapse
- Make informed decisions about treatment modifications
Frequently Asked Questions
What are immunophenotypic abnormalities and how do they help diagnose blood cancers?
Immunophenotypic abnormalities are distinctive patterns of proteins and markers on blood cells that differ from normal cells. They help diagnose blood cancers by providing specific cellular "signatures" that identify different types of leukemia and lymphoma, allowing for precise diagnosis and treatment planning.
How does immunophenotyping by flow cytometry work to detect abnormal cells in leukemia or lymphoma?
Flow cytometry analyzes cells one by one using laser technology and fluorescent markers. The technique identifies specific proteins and markers on cell surfaces, creating detailed profiles of normal and abnormal cells. This helps distinguish cancerous cells from healthy ones based on their unique marker patterns.
What do abnormal immunophenotyping test results mean for my treatment and prognosis?
Abnormal results help determine the exact type of blood cancer present and guide treatment selection. They can indicate which therapies might be most effective, help monitor treatment response, and provide information about potential outcomes. The specific pattern of abnormalities can influence prognosis and treatment planning.
Can immunophenotypic abnormalities change during or after cancer treatment?
Yes, immunophenotypic abnormalities can change during treatment as cancer cells respond to therapy or develop resistance. Regular monitoring of these changes helps doctors assess treatment effectiveness and adjust strategies as needed.
What types of blood or tissue samples are needed for immunophenotyping tests?
Immunophenotyping can be performed on various samples, including peripheral blood, bone marrow aspirates, lymph node tissue, and other affected tissues. The choice of sample depends on the suspected type of cancer and its location in the body.