When using an intrauterine device (IUD) for contraception, it's crucial to understand the different types of bleeding you might experience, including implantation bleeding. While IUDs are highly effective birth control methods, distinguishing between normal bleeding patterns and potential warning signs is essential for your reproductive health.
This comprehensive guide will help you understand what implantation bleeding looks like when you have an IUD, how to identify potential complications, and when to seek medical attention.
Understanding Normal IUD Bleeding Patterns
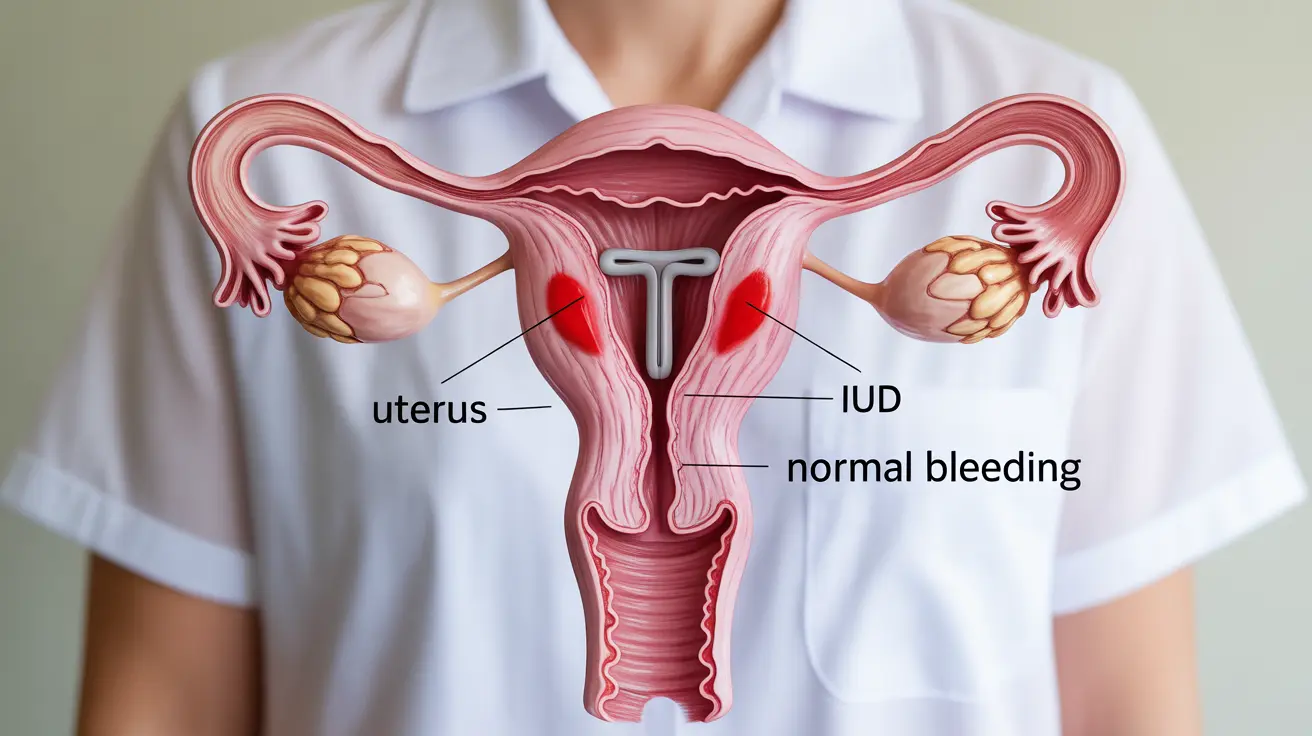
Before discussing implantation bleeding, it's important to understand what constitutes normal bleeding with an IUD:
- Spotting or light bleeding during the first 3-6 months
- Changes in menstrual flow and duration
- Irregular bleeding patterns
- Possible absence of periods (especially with hormonal IUDs)
Recognizing Implantation Bleeding with an IUD
Implantation bleeding while having an IUD is relatively rare but possible. Here's what you should know about its characteristics:
Appearance and Timing
Implantation bleeding typically appears as:
- Light pink or brown spotting
- Much lighter than a normal period
- Lasting 1-3 days
- Occurring about 6-12 days after conception
Warning Signs vs. Normal Bleeding
It's crucial to distinguish between normal bleeding and potentially concerning symptoms:
- Normal bleeding is typically light to moderate
- Warning signs include heavy bleeding, severe cramping, or bright red blood
- Fever or unusual discharge may indicate infection
- Severe abdominal pain requires immediate medical attention
Pregnancy Risks with an IUD
While IUDs are highly effective, pregnancy can still occur in rare cases:
Risk Factors
Certain situations may increase the risk of pregnancy with an IUD:
- Improperly placed IUD
- Expired IUD
- Unnoticed IUD expulsion
- Certain medications that may interfere with effectiveness
Complications and Concerns
If pregnancy occurs with an IUD in place, there are several important considerations:
- Higher risk of ectopic pregnancy
- Increased chance of miscarriage
- Potential infection risks
- Need for immediate medical evaluation
When to Seek Medical Care
Contact your healthcare provider immediately if you experience:
- Heavy bleeding with large clots
- Severe pelvic pain or cramping
- Fever or chills
- Missing IUD strings
- Positive pregnancy test
Frequently Asked Questions
What does implantation bleeding with an IUD look like and how can I tell if it's normal or a problem? Implantation bleeding with an IUD typically appears as light pink or brown spotting that lasts 1-3 days. It's usually much lighter than a normal period. If bleeding becomes heavy, bright red, or is accompanied by severe pain, consult your healthcare provider immediately.
Can I get pregnant while using an IUD, and what are the risks if I experience bleeding during early pregnancy? While rare, pregnancy can occur with an IUD. The risk is less than 1%. If pregnancy occurs and you experience bleeding, seek immediate medical care as there's an increased risk of ectopic pregnancy and other complications.
How can I differentiate between implantation bleeding and bleeding caused by infection or complications related to an IUD? Implantation bleeding is typically light and brief, while infection-related bleeding may be accompanied by fever, unusual discharge, or pelvic pain. Complication-related bleeding tends to be heavier and may include severe cramping or clots.
What should I do if I have vaginal bleeding and pelvic pain while pregnant with an IUD in place? If you experience vaginal bleeding and pelvic pain while pregnant with an IUD, seek emergency medical care immediately. These symptoms could indicate serious complications requiring urgent evaluation.
Is it safer to remove the IUD if I find out I'm pregnant, and what are the possible pregnancy complications if I keep it? Generally, healthcare providers recommend removing the IUD if pregnancy is confirmed and the strings are visible. Keeping the IUD in place during pregnancy increases risks of miscarriage, infection, and preterm delivery. The decision should be made in consultation with your healthcare provider based on your specific situation.