When dealing with potential colon inflammation, medical professionals often turn to CT (computed tomography) scans as a valuable diagnostic tool. This advanced imaging technique can provide detailed insights into the condition of your colon and help healthcare providers make informed decisions about treatment approaches.
Understanding how CT scans work for detecting an inflamed colon and their role in diagnosing conditions like ulcerative colitis is crucial for patients facing these health challenges. Let's explore the capabilities, benefits, and limitations of CT scans in evaluating colon inflammation.
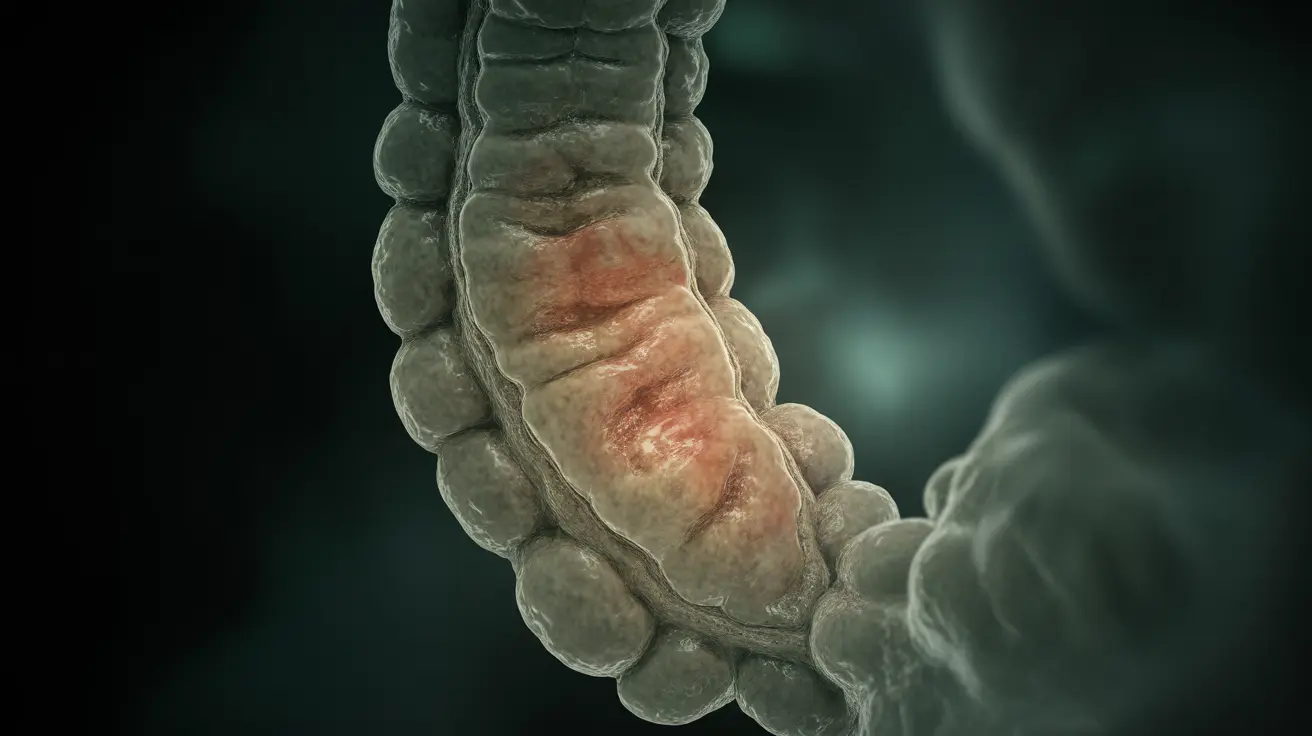
How CT Scans Detect Colon Inflammation
CT scans use X-ray technology and computer processing to create detailed cross-sectional images of the body. When examining an inflamed colon, these scans can reveal several key indicators:
- Thickening of the colon wall
- Changes in surrounding tissue
- Presence of inflammation markers
- Abnormal blood vessel patterns
- Complications such as perforations or abscesses
The Role of Contrast Material
Many CT scans for colon inflammation utilize contrast material, which can be administered orally, rectally, or intravenously. This special dye helps highlight specific areas of the digestive tract, making inflammation and other abnormalities more visible to radiologists.
Advantages of CT Scans for Colon Assessment
CT scans offer several benefits when evaluating colon inflammation:
- Non-invasive examination method
- Quick imaging process
- Ability to view multiple tissue layers
- Detection of complications beyond the colon
- Useful in emergency situations
CT Scans vs. Colonoscopy
While both diagnostic tools are valuable, they serve different purposes in colon assessment. CT scans excel in emergency situations and when looking for complications outside the colon wall. However, colonoscopy remains the gold standard for directly visualizing the colon's inner lining and obtaining tissue samples for definitive diagnosis.
Understanding CT Scan Limitations
CT scans have certain limitations when it comes to colon assessment:
- Cannot provide tissue samples for biopsy
- May miss subtle mucosal changes
- Exposure to radiation
- Less detailed view of the colon's interior
- May not detect early-stage inflammation
Frequently Asked Questions
What signs of an inflamed colon can a CT scan detect in ulcerative colitis?
CT scans can detect wall thickening, increased density of surrounding fat, enlarged lymph nodes, and potential complications like perforations or abscesses in cases of ulcerative colitis. These signs help physicians assess the extent and severity of inflammation.
How does a CT scan with contrast help in evaluating colon inflammation?
Contrast material enhances the visibility of the colon wall and surrounding tissues on CT images. This improved visualization helps doctors better identify areas of inflammation, assess wall thickness, and detect potential complications more accurately.
Can a CT scan definitively diagnose ulcerative colitis or is a colonoscopy necessary?
While CT scans can show signs of inflammation, a colonoscopy with biopsy is typically necessary for a definitive diagnosis of ulcerative colitis. CT scans serve as a complementary diagnostic tool but cannot replace the detailed mucosal examination and tissue sampling provided by colonoscopy.
When is a CT scan preferred over colonoscopy for assessing an inflamed colon?
CT scans are preferred in emergency situations, when patients have severe symptoms that make colonoscopy risky, or when doctors need to evaluate complications that may extend beyond the colon wall. They're also useful for patients who cannot undergo colonoscopy for various medical reasons.
What are the limitations of using a CT scan to diagnose and monitor ulcerative colitis?
CT scans have several limitations: they cannot provide tissue samples, may miss subtle mucosal changes, expose patients to radiation, and may not detect early-stage inflammation. Additionally, they're less effective for routine monitoring of disease activity compared to colonoscopy.