For individuals struggling with obstructive sleep apnea who haven't found success with CPAP therapy, the Inspire device offers an innovative alternative treatment option. Understanding Medicare coverage for this breakthrough technology is crucial for those considering this treatment path.
This comprehensive guide explains how Medicare covers the Inspire device, including eligibility requirements, coverage details, and what you can expect to pay out-of-pocket.
Understanding Medicare Coverage for Inspire
Medicare Part B typically covers the Inspire device when it's deemed medically necessary and when specific eligibility criteria are met. The coverage includes both the surgical implantation procedure and the device itself when performed in an outpatient setting.
Medicare Part B Coverage Requirements
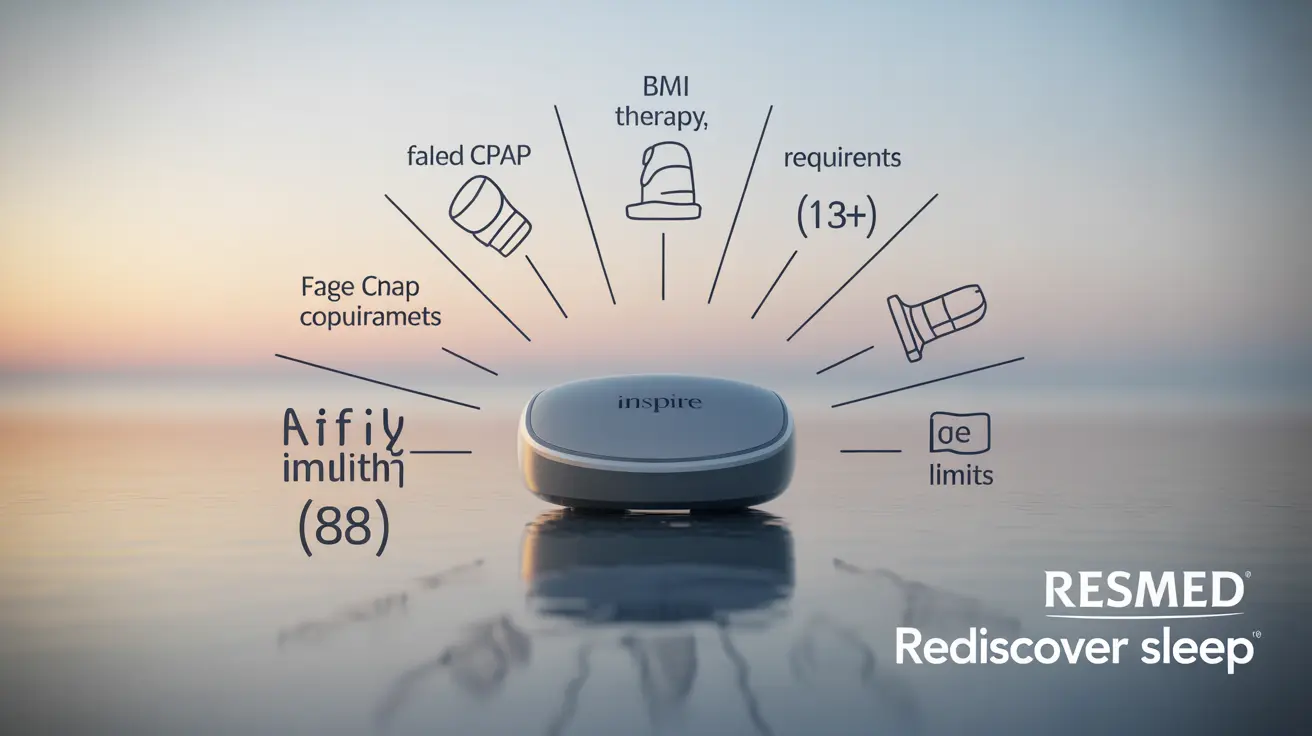
To qualify for Medicare coverage of the Inspire device, patients must meet several specific criteria:
- Diagnosed with moderate to severe obstructive sleep apnea
- Failed or cannot tolerate CPAP therapy
- Body Mass Index (BMI) of less than 35
- Age 18 or older
- Meet specific sleep study criteria
- No anatomical findings that would block upper airway stimulation
CPAP Trial Requirement Explained
Medicare requires patients to try CPAP or BiPAP therapy before approving coverage for the Inspire device. This requirement exists because:
- CPAP is considered the first-line treatment for sleep apnea
- It's generally less invasive than surgical options
- It's typically more cost-effective
- Many patients achieve successful results with CPAP therapy
Cost Considerations Under Original Medicare
Under Original Medicare Part B, patients are typically responsible for:
- 20% of the Medicare-approved amount for the device
- The Part B deductible (if not already met)
- Any applicable facility fees
- Coinsurance for follow-up visits and adjustments
Additional Cost Factors
The total out-of-pocket costs can vary based on:
- Whether you have supplemental insurance
- The specific facility where the procedure is performed
- Any additional medical services required
- Post-procedure care and adjustments
Medicare Advantage Coverage
Medicare Advantage plans must provide at least the same level of coverage as Original Medicare, but coverage details can vary. Some plans may offer additional benefits or have different cost-sharing structures.
Checking Your Plan's Coverage
To verify coverage under your Medicare Advantage plan:
- Contact your plan directly
- Review your plan's Evidence of Coverage document
- Speak with your plan's customer service representative
- Consult with your healthcare provider's billing department
Frequently Asked Questions
Does Medicare Part B cover the Inspire device for treating obstructive sleep apnea? Yes, Medicare Part B covers the Inspire device when medical necessity criteria are met and the procedure is performed in an outpatient setting.
What eligibility requirements must I meet for Medicare to cover the Inspire sleep apnea implant? You must have moderate to severe sleep apnea, have tried and failed CPAP therapy, maintain a BMI under 35, be 18 or older, and meet specific sleep study criteria.
Why do I need to try CPAP or BiPAP therapy before Medicare will cover the Inspire device? Medicare requires a CPAP trial first because it's considered the standard first-line treatment, is less invasive, and is often effective for managing sleep apnea.
How much will I have to pay out-of-pocket for Inspire therapy under Original Medicare? Under Original Medicare, you're responsible for 20% of the Medicare-approved amount plus your Part B deductible if not already met. Additional costs may include facility fees and follow-up care.
Do Medicare Advantage plans cover the Inspire device, and how can I check my specific plan's coverage? Medicare Advantage plans must provide at least the same coverage as Original Medicare. Contact your plan directly or review your Evidence of Coverage document to verify specific coverage details and costs.