Intermittent complete heart block is a serious cardiac conduction disorder that occurs when the electrical signals between the heart's upper chambers (atria) and lower chambers (ventricles) are temporarily but completely blocked. Unlike permanent complete heart block, this condition comes and goes unpredictably, making it particularly challenging to diagnose and manage.
This intermittent disruption in the heart's electrical system can lead to dangerous drops in heart rate and potentially life-threatening complications. Understanding the warning signs, risk factors, and treatment options is crucial for anyone who may be at risk for this condition or experiencing unexplained cardiac symptoms.
What Causes Intermittent Complete Heart Block?
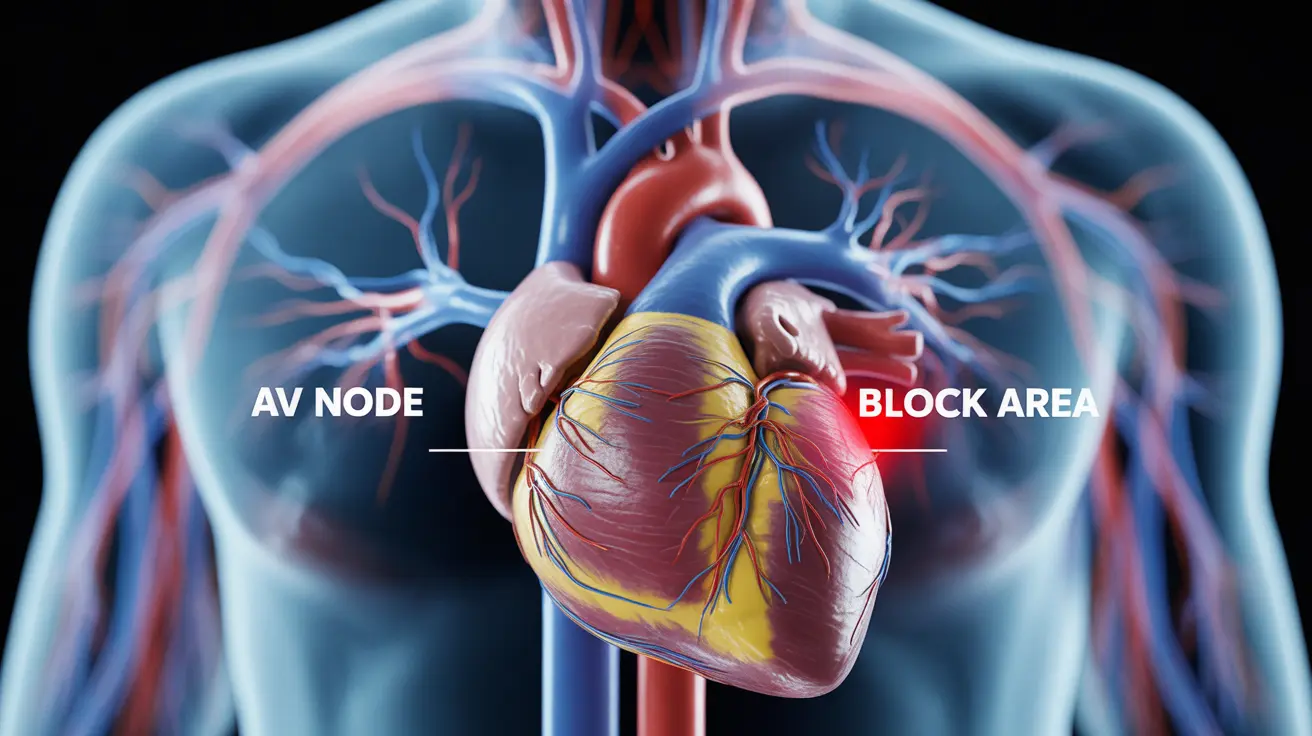
Several underlying conditions and factors can trigger episodes of intermittent complete heart block. The most common causes involve damage or dysfunction to the heart's electrical conduction system, particularly the atrioventricular (AV) node and surrounding pathways.
Coronary artery disease stands as one of the leading culprits, as reduced blood flow to the heart muscle can damage the delicate electrical pathways. Heart attacks, especially those affecting the inferior wall of the heart, frequently result in conduction abnormalities that may manifest as intermittent complete heart block.
Certain medications pose significant risks for developing this condition. Beta-blockers, calcium channel blockers, and digoxin can slow electrical conduction through the AV node, potentially causing temporary complete blocks in susceptible individuals. Electrolyte imbalances, particularly low potassium or magnesium levels, can also disrupt normal electrical conduction.
Risk Factors and Vulnerable Populations
Age represents a primary risk factor, as the heart's electrical system naturally deteriorates over time. Adults over 65 face increased vulnerability, especially those with existing cardiovascular conditions. Men appear to develop intermittent complete heart block slightly more frequently than women, though the difference becomes less pronounced with advancing age.
Individuals with structural heart disease, including cardiomyopathy, valve disorders, or congenital heart defects, carry elevated risks. Previous cardiac procedures, such as valve replacement surgery or catheter ablations, may inadvertently damage conduction pathways, leading to intermittent blocks.
Certain inflammatory conditions, including Lyme disease, rheumatic fever, and sarcoidosis, can infiltrate and damage the heart's electrical system. Athletes who engage in intense endurance training may also develop heightened vagal tone, which can occasionally trigger episodes in predisposed individuals.
Recognizing Warning Signs and Symptoms
The symptoms of intermittent complete heart block can vary dramatically depending on the duration and frequency of episodes. During active blocks, patients typically experience a sudden, dramatic drop in heart rate, often falling below 40 beats per minute.
Dizziness and lightheadedness represent the most common initial symptoms, occurring as blood flow to the brain temporarily decreases. Many patients describe feeling faint or experiencing near-fainting episodes, particularly when standing up quickly or during physical exertion.
Fatigue and weakness often develop gradually, especially if episodes become more frequent or prolonged. Some individuals report chest discomfort or pressure, though this isn't universal. In severe cases, patients may experience brief episodes of confusion, memory problems, or even temporary loss of consciousness.
Diagnostic Approaches and Monitoring Methods
Diagnosing intermittent complete heart block requires patience and sophisticated monitoring techniques, as episodes may not occur during routine medical visits. Standard electrocardiograms (ECGs) provide valuable baseline information but often miss intermittent events.
Holter monitors, which record heart rhythms continuously for 24-48 hours, offer improved detection rates for patients experiencing frequent episodes. For those with less frequent symptoms, event monitors or implantable loop recorders may be necessary to capture sporadic occurrences over weeks or months.
Electrophysiology studies represent the gold standard for definitive diagnosis in complex cases. During these procedures, cardiologists use specialized catheters to map the heart's electrical system and can sometimes trigger episodes under controlled conditions, allowing for precise localization of conduction problems.
Treatment Strategies and Management Options
Treatment approaches for intermittent complete heart block depend heavily on symptom severity, episode frequency, and underlying causes. For patients experiencing significant symptoms or dangerous drops in heart rate, permanent pacemaker implantation often becomes necessary.
Modern dual-chamber pacemakers can detect when complete heart block occurs and immediately provide backup pacing to maintain adequate heart rates. These devices offer sophisticated programming options that can adapt to individual patient needs and activity levels.
In cases where medications trigger episodes, careful adjustment or substitution of offending drugs may resolve the problem entirely. Electrolyte corrections, particularly addressing potassium or magnesium deficiencies, can prevent future episodes in some patients.
For individuals with underlying inflammatory conditions, treating the root cause with appropriate anti-inflammatory medications or antibiotics may improve conduction abnormalities and reduce episode frequency.
Lifestyle Modifications and Prevention Strategies
While not all cases of intermittent complete heart block can be prevented, several lifestyle modifications may help reduce episode frequency and severity. Maintaining optimal cardiovascular health through regular exercise, healthy diet choices, and weight management supports overall heart function.
Avoiding excessive alcohol consumption and eliminating tobacco use can improve heart health and reduce the risk of developing additional cardiac conditions that might worsen conduction problems. Staying properly hydrated and maintaining balanced electrolyte levels through adequate nutrition also plays a supportive role.
Patients should work closely with their healthcare providers to monitor and adjust medications that might affect heart rhythm. Regular follow-up appointments allow for early detection of worsening symptoms and timely treatment adjustments.
Frequently Asked Questions
What are the common causes and risk factors of intermittent complete heart block?
Common causes include coronary artery disease, heart attacks, certain medications (particularly beta-blockers and calcium channel blockers), electrolyte imbalances, and structural heart disease. Risk factors encompass advanced age, male gender, existing cardiovascular conditions, inflammatory diseases like Lyme disease, and previous cardiac procedures. Athletes with high vagal tone may also be at increased risk.
What symptoms should prompt me to seek immediate medical attention for complete heart block?
Seek emergency care immediately if you experience fainting or near-fainting episodes, severe dizziness with slow heart rate, chest pain accompanied by weakness, sudden confusion or memory problems, or any episode where you lose consciousness. Additionally, if you have a known heart condition and experience new onset fatigue, weakness, or breathing difficulties, contact your healthcare provider promptly.
How is intermittent complete heart block diagnosed and monitored by doctors?
Diagnosis typically involves electrocardiograms (ECGs), though these may miss intermittent episodes. Extended monitoring with Holter monitors (24-48 hours), event monitors, or implantable loop recorders helps capture sporadic events. Electrophysiology studies provide definitive diagnosis in complex cases by mapping the heart's electrical system and sometimes triggering episodes under controlled conditions.
What treatment options are available for managing intermittent complete heart block?
Treatment options include permanent pacemaker implantation for patients with significant symptoms, medication adjustments to eliminate triggering drugs, electrolyte corrections, and treatment of underlying inflammatory conditions. Dual-chamber pacemakers represent the most common definitive treatment, providing backup pacing when complete heart block occurs.
Can lifestyle changes or medication adjustments prevent or reduce episodes of intermittent complete heart block?
Yes, several approaches may help reduce episodes. These include eliminating or adjusting medications that slow heart conduction, correcting electrolyte imbalances, treating underlying inflammatory conditions, maintaining cardiovascular health through exercise and proper nutrition, avoiding excessive alcohol and tobacco, and staying properly hydrated. However, many patients ultimately require pacemaker implantation for definitive management.