Many people wonder about the relationship between alcohol consumption and blood thinning, especially those taking anticoagulant medications. While alcohol can impact blood clotting mechanisms, its effects are complex and potentially dangerous when combined with prescribed blood thinners.
This comprehensive guide explores how alcohol affects blood coagulation, its interactions with blood-thinning medications, and important safety considerations for those on anticoagulant therapy.
How Alcohol Affects Blood Clotting
Alcohol can temporarily affect your body's blood-clotting mechanisms in several ways. It reduces the production of blood-clotting proteins in your liver and decreases the function of platelets, the blood cells responsible for forming clots. However, this doesn't make alcohol a safe or reliable blood thinner.
Unlike prescribed anticoagulants, alcohol's effects on blood clotting are unpredictable and can vary significantly based on consumption patterns and individual factors.
Alcohol and Prescription Blood Thinners
Common Blood-Thinning Medications
Several types of prescription blood thinners are commonly used in medical treatment:
- Warfarin (Coumadin)
- Direct oral anticoagulants (DOACs)
- Heparin
- Low-molecular-weight heparin
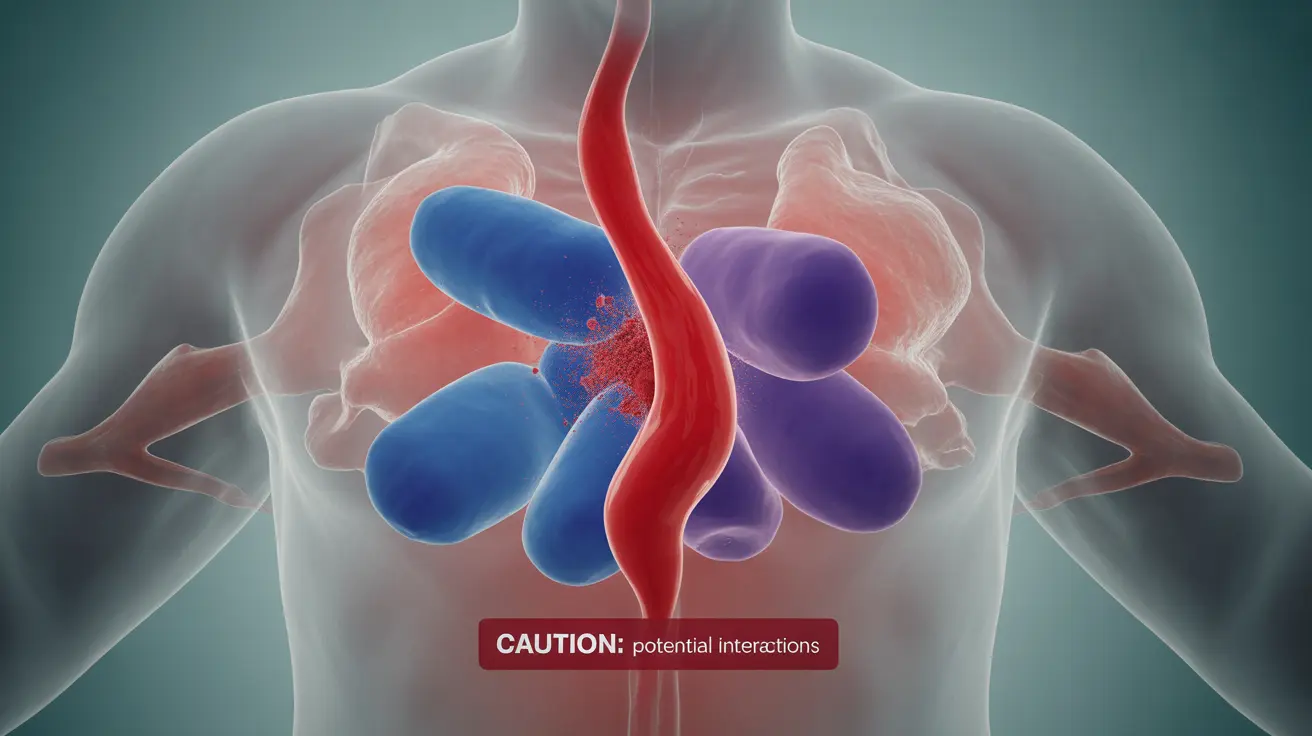
Dangerous Interactions
Combining alcohol with prescription blood thinners can lead to serious complications. Alcohol can enhance the blood-thinning effects of these medications, potentially leading to dangerous bleeding episodes. Additionally, alcohol can interfere with the metabolism of certain blood thinners, making their effects less predictable.
Safe Consumption Guidelines
If you're taking blood thinners, it's crucial to follow these safety guidelines regarding alcohol consumption:
- Consult your healthcare provider about alcohol use
- Never exceed recommended drinking limits
- Maintain consistent drinking patterns if you choose to drink
- Consider avoiding alcohol completely while on anticoagulation therapy
Warning Signs and Risk Factors
When taking blood thinners, certain symptoms may indicate dangerous bleeding complications, especially if combined with alcohol:
- Unusual bruising or bleeding
- Persistent headaches
- Dizziness
- Blood in urine or stool
- Severe stomach pain
- Vomiting blood
Frequently Asked Questions
Is alcohol really a blood thinner and how does it affect blood clotting?
Alcohol has temporary blood-thinning effects by reducing platelet function and decreasing the production of blood-clotting proteins in the liver. However, it's not a reliable or safe blood thinner compared to prescribed medications.
Can drinking alcohol increase the risk of bleeding when I am taking blood thinner medications?
Yes, combining alcohol with blood thinners can significantly increase bleeding risks by enhancing the anticoagulant effects of the medication and potentially interfering with its metabolism in your body.
How much alcohol is safe to drink if I am on a blood thinner prescription?
The safe amount varies by individual and specific medication. Many healthcare providers recommend limiting or avoiding alcohol entirely while on blood thinners. Always consult your doctor for personalized guidance.
Why does heavy alcohol use increase the risk of stroke and bleeding despite some blood-thinning effects?
Heavy alcohol use can paradoxically increase both bleeding and clotting risks. While it thins blood temporarily, it can also lead to inflammation, liver damage, and irregular heart rhythms that increase stroke risk.
What symptoms should I watch for that indicate dangerous bleeding when mixing alcohol with blood thinners?
Watch for unusual bruising, persistent headaches, blood in urine or stool, excessive bleeding from minor cuts, unexplained dizziness, and severe stomach pain. Seek immediate medical attention if these symptoms occur.