The relationship between diabetes and autoimmune responses has long intrigued medical researchers and healthcare providers. While it's widely known that Type 1 diabetes is an autoimmune condition, the role of autoimmunity in Type 2 diabetes is more complex and continues to be an active area of scientific investigation.
Understanding the autoimmune aspects of different types of diabetes is crucial for both proper diagnosis and treatment. This comprehensive guide explores the autoimmune connections in diabetes and their implications for patient care.
The Autoimmune Nature of Type 1 Diabetes
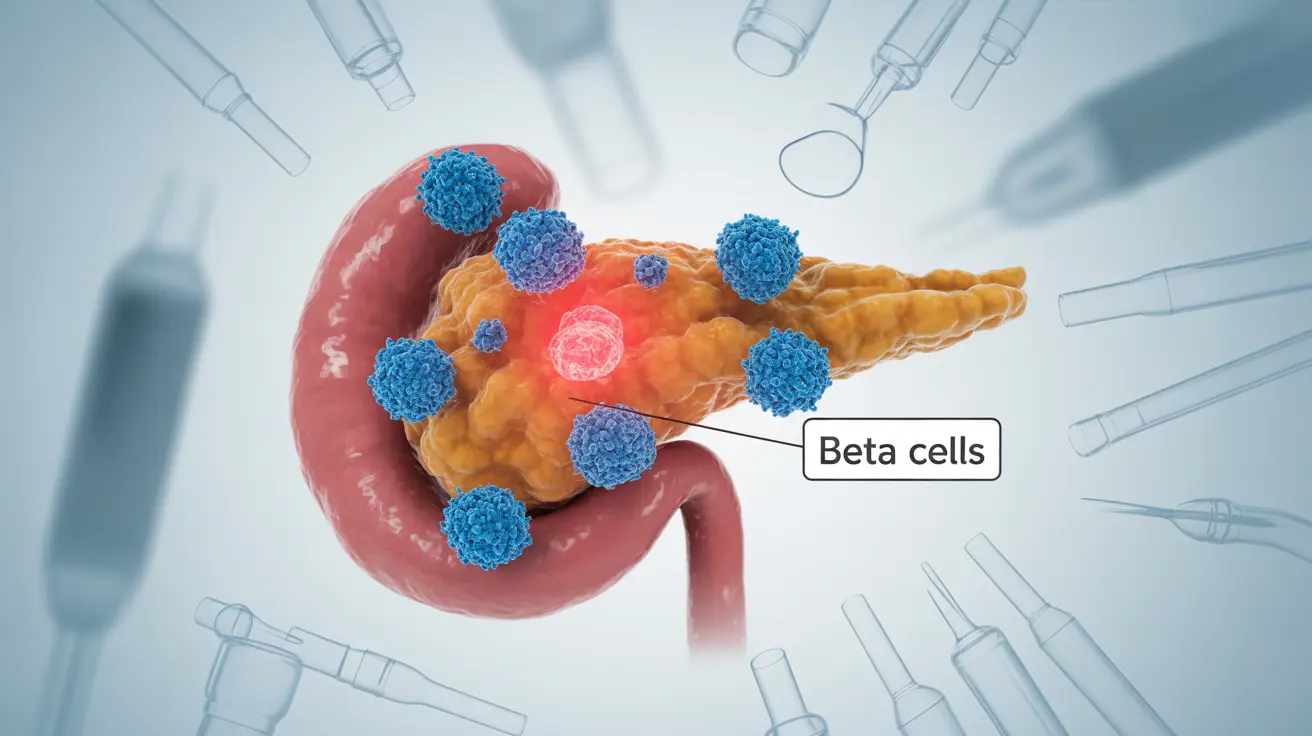
Type 1 diabetes is definitively classified as an autoimmune disease. In this condition, the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This autoimmune response results in the body's inability to produce insulin, leading to the need for lifelong insulin therapy.
The autoimmune attack in Type 1 diabetes typically occurs early in life, though it can develop at any age. Specific antibodies targeting pancreatic cells can be detected in blood tests, confirming the autoimmune nature of the condition.
Type 2 Diabetes: Beyond Simple Metabolic Disorder
Traditional understanding categorizes Type 2 diabetes as primarily a metabolic disorder characterized by insulin resistance and impaired insulin production. However, recent research suggests that inflammatory and autoimmune mechanisms may play more significant roles than previously thought.
The Role of Inflammation and Immune Response
Studies have shown that chronic inflammation, which involves immune system activation, contributes to the development and progression of Type 2 diabetes. This inflammatory response can affect insulin sensitivity and beta cell function, creating a complex interaction between metabolism and immunity.
Emerging Evidence of Autoimmune Components
Research has identified specific immune markers and autoantibodies in some individuals with Type 2 diabetes, suggesting that autoimmune reactions might contribute to the condition's development in certain cases. This has led to the concept of "hybrid" diabetes, where both metabolic and autoimmune factors are present.
Treatment Approaches and Immune Considerations
Current treatment strategies for Type 2 diabetes primarily focus on managing blood glucose levels through medication, diet, and lifestyle modifications. However, the growing understanding of immune system involvement has opened new avenues for therapeutic approaches.
Conventional Treatments
- Oral medications to improve insulin sensitivity
- Injectable medications like GLP-1 receptor agonists
- Lifestyle modifications including diet and exercise
- Blood glucose monitoring and management
Emerging Therapeutic Directions
The recognition of immune system involvement has led to research into immune-modulating therapies for certain cases of Type 2 diabetes. These approaches aim to address both the metabolic and potential autoimmune aspects of the condition.
Frequently Asked Questions
Is type 1 diabetes an autoimmune disease, and how does it differ from type 2 diabetes?
Yes, Type 1 diabetes is definitively an autoimmune disease where the immune system destroys insulin-producing cells. Type 2 diabetes traditionally isn't classified as autoimmune, but rather as a metabolic disorder involving insulin resistance and decreased insulin production. The onset, treatment approaches, and underlying mechanisms differ significantly between the two types.
Can type 2 diabetes involve autoimmune reactions, or is it strictly a metabolic disorder?
Recent research suggests that Type 2 diabetes can involve autoimmune components in some cases, though it's primarily a metabolic disorder. Some patients show evidence of autoimmune markers, indicating a more complex disease process than previously understood.
What are the current treatments for type 2 diabetes, and could immune-modulating therapies be effective?
Current treatments focus on medication, lifestyle changes, and blood sugar management. While immune-modulating therapies are not standard treatment, research into their potential effectiveness is ongoing, especially for cases showing autoimmune characteristics.
How do autoimmune responses contribute to the development or progression of type 2 diabetes?
Autoimmune responses can contribute through chronic inflammation and potential direct damage to insulin-producing cells. This immune system involvement may accelerate the progression of insulin resistance and beta cell dysfunction in some individuals.
Are there specific symptoms or markers that indicate type 2 diabetes has an autoimmune component?
Certain blood tests can detect autoantibodies and inflammatory markers that might indicate an autoimmune component. However, these tests aren't routinely performed in Type 2 diabetes diagnosis unless there are specific clinical indicators suggesting autoimmune involvement.