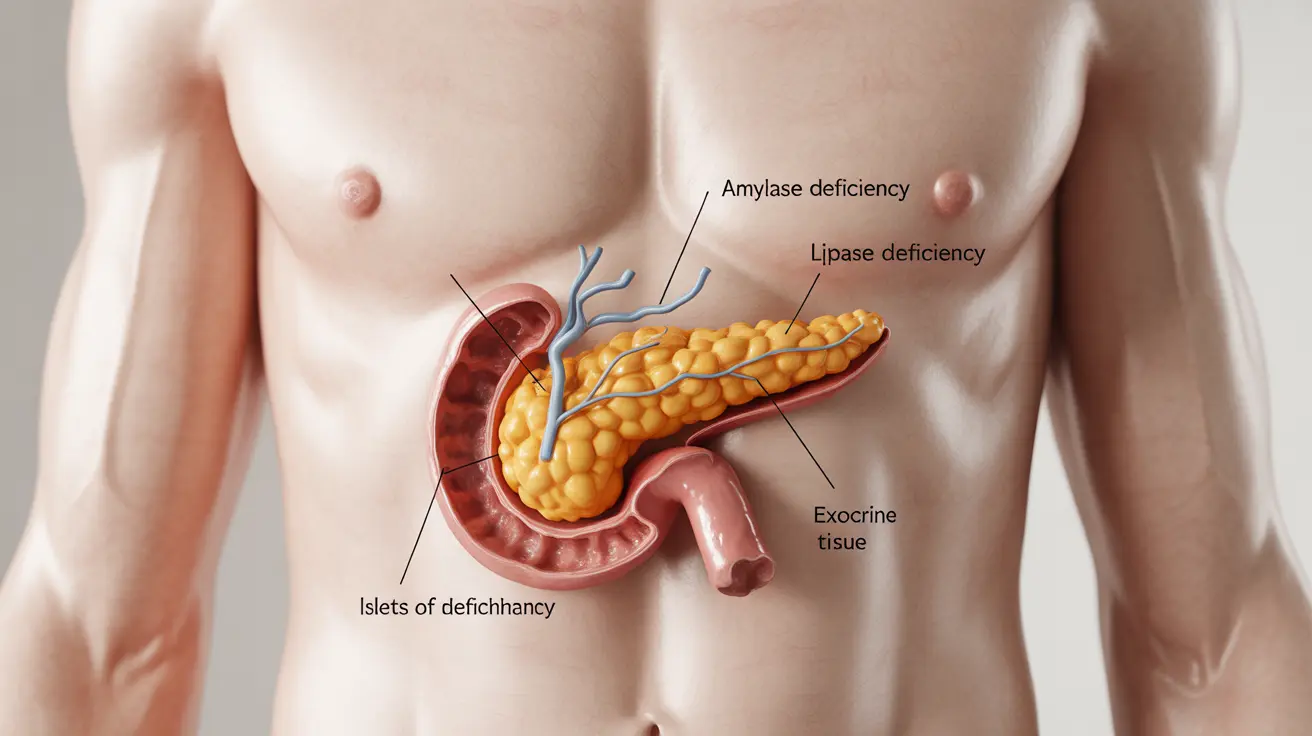
Exocrine pancreatic insufficiency (EPI) is a complex digestive condition that affects the pancreas's ability to produce essential digestive enzymes. While many people wonder about its connection to autoimmune diseases, it's important to understand that EPI itself is not primarily an autoimmune condition, though it can be related to or caused by autoimmune disorders in some cases.
This comprehensive guide will explore the relationship between EPI and autoimmune conditions, its various causes, and how it's managed effectively.
The Relationship Between EPI and Autoimmune Conditions
While EPI isn't inherently an autoimmune disease, it can develop as a consequence of certain autoimmune conditions. The primary distinction lies in the mechanism of how pancreatic function becomes impaired. In autoimmune conditions, the body's immune system mistakenly attacks its own tissues, while EPI can occur through various mechanisms, both autoimmune and non-autoimmune.
Primary Causes of EPI
Several conditions and factors can lead to the development of EPI:
- Chronic pancreatitis
- Cystic fibrosis
- Pancreatic cancer
- Previous pancreatic surgery
- Diabetes (particularly type 1)
- Autoimmune pancreatitis
Diagnosis and Testing Methods
Diagnosing EPI involves several key steps and tests:
- Fecal elastase tests
- Blood tests for nutritional deficiencies
- Imaging studies of the pancreas
- Symptom evaluation and medical history review
Treatment Approaches for EPI
Management of EPI typically involves a multi-faceted approach:
Enzyme Replacement Therapy
Pancreatic enzyme replacement therapy (PERT) is the cornerstone of EPI treatment, helping to restore normal digestive function and nutrient absorption.
Dietary Modifications
Specific dietary changes can significantly improve symptoms and quality of life for people with EPI:
- Small, frequent meals
- Proper timing of enzyme supplements
- Balanced nutrient intake
- Adequate fat consumption with enzyme support
Lifestyle Management Strategies
Successfully managing EPI often requires certain lifestyle adjustments:
- Regular monitoring of nutritional status
- Avoiding alcohol and tobacco
- Maintaining proper medication schedules
- Working closely with healthcare providers
Frequently Asked Questions
Is exocrine pancreatic insufficiency (EPI) considered an autoimmune disease?
No, EPI itself is not an autoimmune disease. While it can be caused by autoimmune conditions like autoimmune pancreatitis, EPI is primarily a condition where the pancreas doesn't produce enough digestive enzymes, regardless of the underlying cause.
What are the most common causes of exocrine pancreatic insufficiency besides autoimmune conditions?
The most common non-autoimmune causes of EPI include chronic pancreatitis, cystic fibrosis, pancreatic cancer, pancreatic surgery, and severe cases of diabetes. These conditions can damage or impair pancreatic function directly.
How is exocrine pancreatic insufficiency diagnosed and treated?
EPI is diagnosed through a combination of fecal elastase tests, blood tests, imaging studies, and symptom evaluation. Treatment primarily involves pancreatic enzyme replacement therapy (PERT), dietary modifications, and lifestyle changes.
Can autoimmune diseases like autoimmune pancreatitis lead to exocrine pancreatic insufficiency?
Yes, autoimmune pancreatitis can lead to EPI by causing inflammation and damage to the pancreas. This damage can impair the organ's ability to produce sufficient digestive enzymes.
What lifestyle changes and dietary adjustments help manage symptoms of exocrine pancreatic insufficiency?
Key lifestyle and dietary adjustments include eating smaller, more frequent meals, timing enzyme supplements correctly with meals, maintaining a balanced diet with adequate fat intake, avoiding alcohol and tobacco, and regular nutritional monitoring with healthcare providers.