Hypothyroidism is a complex condition affecting millions of Americans, and many wonder if it's an autoimmune disease. While autoimmune disorders are indeed a leading cause of hypothyroidism, the relationship between these conditions requires careful explanation to understand fully.
In this comprehensive guide, we'll explore the connection between autoimmune diseases and hypothyroidism, examining various causes, symptoms, and treatment approaches to help you better understand this important health topic.
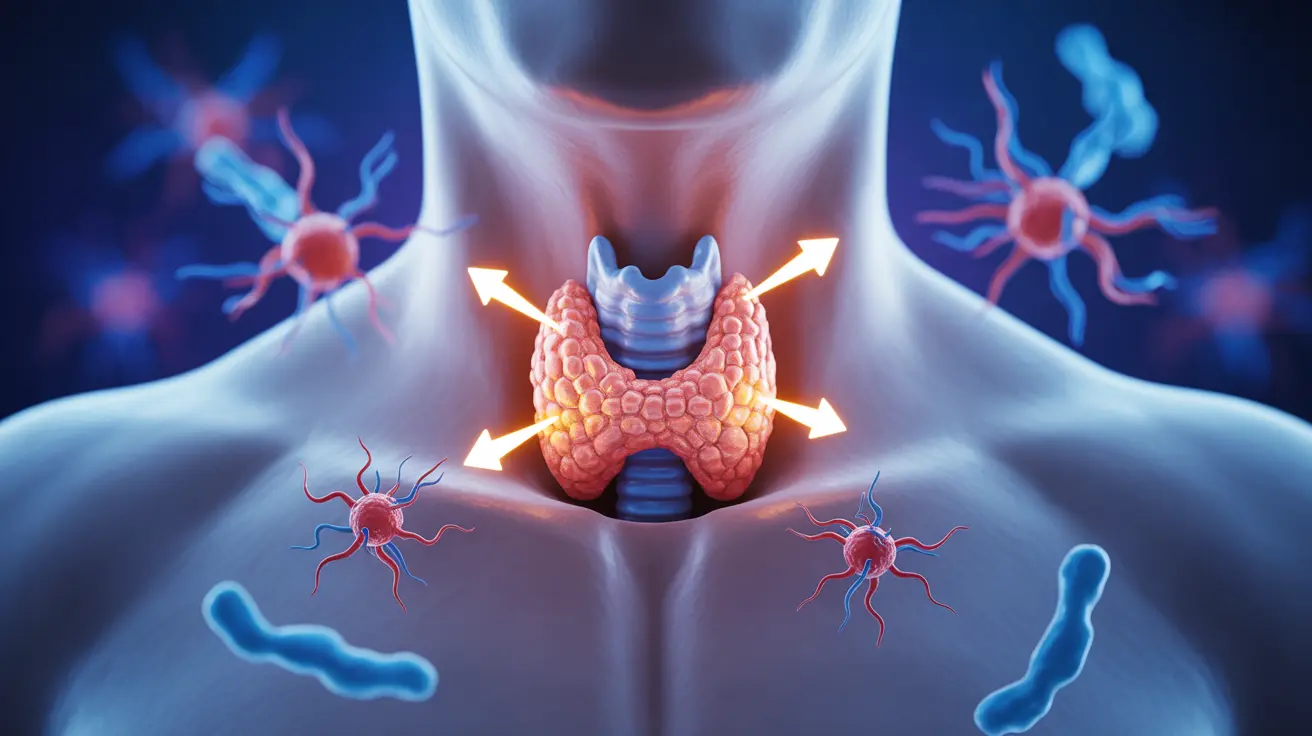
The Autoimmune Connection to Hypothyroidism
The most common cause of hypothyroidism in developed countries is actually an autoimmune condition called Hashimoto's thyroiditis. This condition occurs when the body's immune system mistakenly attacks the thyroid gland, gradually reducing its ability to produce essential hormones.
However, it's important to note that not all cases of hypothyroidism are autoimmune in nature. Understanding this distinction can help guide proper diagnosis and treatment approaches.
Common Symptoms of Autoimmune Hypothyroidism
Autoimmune hypothyroidism typically develops gradually, with symptoms that may include:
- Fatigue and weakness
- Unexplained weight gain
- Cold sensitivity
- Dry skin and brittle nails
- Depression or mood changes
- Memory problems
- Joint and muscle pain
- Heavy or irregular menstrual periods
Non-Autoimmune Causes of Hypothyroidism
Several other factors can lead to hypothyroidism without involving autoimmune responses:
- Surgical removal of the thyroid
- Radiation therapy to the neck area
- Certain medications
- Iodine deficiency
- Congenital conditions
- Pregnancy-related thyroid dysfunction
Risk Factors for Autoimmune Hypothyroidism
Certain individuals may face a higher risk of developing autoimmune hypothyroidism. Key risk factors include:
- Being female
- Family history of thyroid disorders
- Age (more common in middle-aged adults)
- Having other autoimmune conditions
- Recent pregnancy
- Radiation exposure to the neck area
Diagnosis and Treatment Approaches
Proper diagnosis involves blood tests to measure thyroid hormone levels and detect specific antibodies associated with autoimmune thyroid conditions. Treatment typically includes thyroid hormone replacement therapy, regardless of whether the cause is autoimmune or not.
Management Strategies
Effective management of autoimmune hypothyroidism often requires:
- Regular monitoring of thyroid hormone levels
- Consistent medication schedules
- Lifestyle modifications
- Proper nutrition
- Stress management
- Regular exercise
- Adequate sleep
Frequently Asked Questions
Is hypothyroidism always caused by an autoimmune disease like Hashimoto's thyroiditis?
No, while Hashimoto's thyroiditis is the most common cause of hypothyroidism in developed countries, there are several other non-autoimmune causes, including surgical removal of the thyroid, radiation therapy, and certain medications.
What are the common symptoms that indicate autoimmune hypothyroidism?
Common symptoms include fatigue, weight gain, cold sensitivity, dry skin, depression, memory issues, and muscle weakness. These symptoms typically develop gradually over time.
How is hypothyroidism from Hashimoto's disease treated and managed?
Treatment primarily involves thyroid hormone replacement therapy, typically with levothyroxine. Regular monitoring of thyroid levels, consistent medication schedules, and lifestyle modifications are essential components of management.
What other causes besides autoimmune disease can lead to hypothyroidism?
Other causes include thyroid surgery, radiation therapy, certain medications, iodine deficiency, congenital conditions, and pregnancy-related thyroid dysfunction.
Who is at higher risk of developing autoimmune hypothyroidism such as Hashimoto's thyroiditis?
Women, particularly middle-aged adults, those with a family history of thyroid disorders, individuals with other autoimmune conditions, and those who have recently been pregnant are at higher risk. Environmental factors and radiation exposure can also increase risk.