Understanding the genetic aspects of osteoporosis can help you better assess your risk and take proactive steps toward maintaining bone health. While lifestyle factors play a crucial role, genetics significantly influence how likely you are to develop this bone-weakening condition. Recent scientific research has revealed important connections between our genes and bone density, helping healthcare providers better identify and treat those at risk.
This comprehensive guide explores the hereditary nature of osteoporosis, examining how genetics shape your bone health and what you can do to protect yourself, even if you have a family history of the condition.
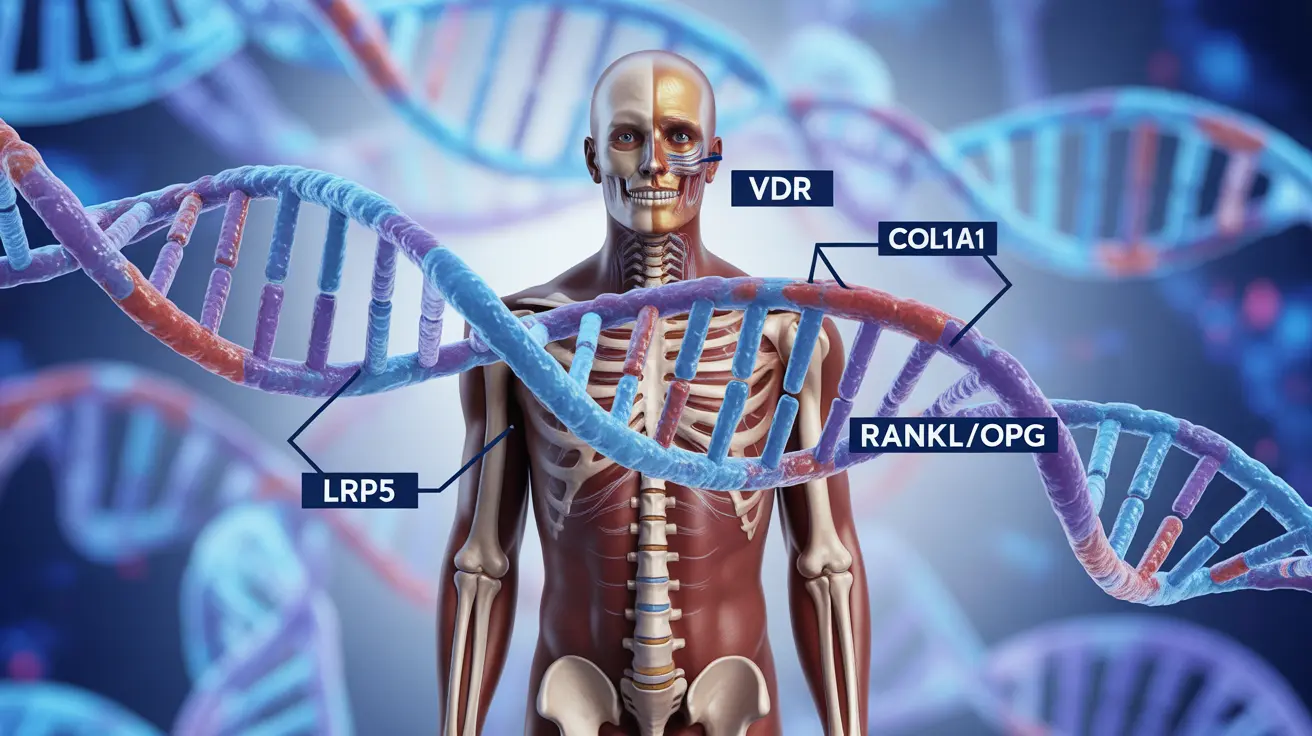
The Role of Genetics in Osteoporosis Development
Research shows that genetics can account for up to 80% of your bone mass potential. Multiple genes work together to regulate bone formation, mineral density, and the rate of bone turnover. Understanding this genetic component is crucial for early intervention and prevention strategies.
Key Genetic Factors
Several specific genes have been identified as playing important roles in bone health and osteoporosis risk:
- VDR (Vitamin D Receptor) gene
- COL1A1 (Collagen Type I) gene
- LRP5 (Low-density lipoprotein receptor-related protein 5) gene
- RANKL and OPG genes
These genes influence various aspects of bone metabolism, from calcium absorption to bone formation and breakdown processes. Variations in these genes can significantly impact your likelihood of developing osteoporosis.
Family History and Risk Assessment
Having a close relative with osteoporosis can significantly increase your risk of developing the condition. This is particularly true if you have a parent or sibling who has been diagnosed with osteoporosis or has experienced fragility fractures.
Understanding Your Family Risk
Key factors to consider when assessing family-related risk include:
- History of fractures in first-degree relatives
- Early menopause in female relatives
- Family pattern of low bone density
- History of height loss or spinal curvature
Prevention Strategies for Those with Genetic Risk
While you cannot change your genetic makeup, you can take several steps to minimize your risk of developing osteoporosis, even with a genetic predisposition:
Lifestyle Modifications
Essential preventive measures include:
- Regular weight-bearing exercise
- Adequate calcium and vitamin D intake
- Maintaining a healthy body weight
- Avoiding smoking and excessive alcohol consumption
- Regular bone density monitoring
Screening and Early Detection
Early screening is crucial for individuals with genetic risk factors. Regular bone density scans can help detect bone loss before it becomes severe, allowing for timely intervention and treatment.
Frequently Asked Questions
Is osteoporosis inherited and how much does genetics affect my risk of developing it?
Yes, osteoporosis has a strong genetic component, with heredity accounting for up to 80% of bone mass potential. However, the actual development of the condition depends on both genetic and environmental factors.
What specific genes are linked to osteoporosis and how do they influence bone health?
Several genes, including VDR, COL1A1, LRP5, and RANKL/OPG, are linked to osteoporosis. These genes regulate various aspects of bone metabolism, including calcium absorption, bone formation, and bone density maintenance.
How does having a family history of osteoporosis or fractures impact my chances of getting the disease?
Having a first-degree relative with osteoporosis significantly increases your risk. If a parent or sibling has osteoporosis or has experienced fragility fractures, your risk may be 2-4 times higher than someone without this family history.
Can lifestyle changes reduce osteoporosis risk even if I have a genetic predisposition?
Yes, lifestyle modifications can significantly reduce your risk despite genetic predisposition. Regular exercise, proper nutrition, and healthy habits can help maintain bone strength and slow bone loss, even in those with genetic risk factors.
When should someone with a family history of osteoporosis get screened for low bone density?
Those with a family history should consider getting their first bone density scan earlier than the general recommendation of age 65. Women should typically start screening at menopause if they have family risk factors, while men should discuss appropriate screening timing with their healthcare provider based on their individual risk factors.