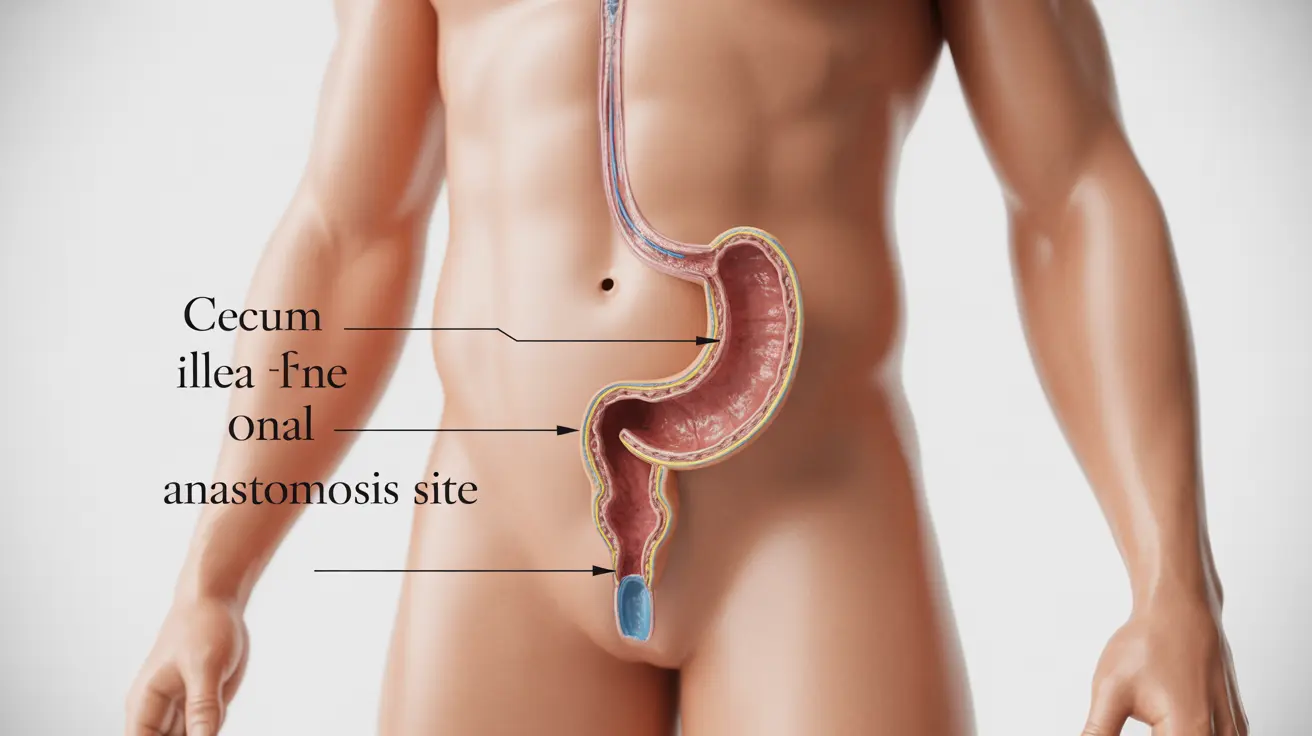
For individuals with ulcerative colitis or familial adenomatous polyposis who undergo J-pouch surgery, understanding the long-term outlook becomes a crucial concern. This innovative surgical procedure, also known as ileal pouch-anal anastomosis (IPAA), offers patients the opportunity to maintain bowel continuity while removing diseased tissue. However, questions about durability, complications, and overall life expectancy after J-pouch surgery naturally arise as patients consider this major surgical intervention.
The decision to undergo J-pouch surgery represents a significant turning point in managing chronic digestive conditions. While the procedure can dramatically improve quality of life for many patients, it's essential to understand both the potential benefits and long-term considerations that may impact your health journey. This comprehensive guide explores the realistic expectations, success rates, and factors that influence outcomes following J-pouch surgery.
Understanding J-Pouch Surgery Longevity
The lifespan of a J-pouch varies considerably among patients, with multiple factors influencing its long-term durability. Research indicates that most J-pouches can function effectively for decades, with many patients experiencing 20-30 years or more of successful pouch function. However, the actual longevity depends on several critical factors including surgical technique, patient age at the time of surgery, underlying condition, and adherence to post-operative care protocols.
Studies tracking long-term outcomes show that approximately 85-90% of J-pouches remain functional after 10 years, while roughly 80-85% continue working effectively after 20 years. These statistics demonstrate that while some pouches may require revision or eventual removal, the majority provide lasting benefits for patients who undergo the procedure.
The construction quality of the initial surgery plays a vital role in determining pouch longevity. Experienced colorectal surgeons who specialize in pouch procedures typically achieve better long-term outcomes, emphasizing the importance of choosing a skilled surgical team for this complex operation.
Success Rates and Complications
J-pouch surgery demonstrates impressive success rates, with studies showing that approximately 90-95% of patients achieve satisfactory functional outcomes without major complications. This high success rate makes the procedure an attractive option for appropriate candidates seeking to avoid permanent colostomy while managing their underlying condition effectively.
However, like any major surgical procedure, J-pouch surgery carries inherent risks. Common complications that may arise include pouchitis (inflammation of the pouch), occurring in roughly 40-50% of patients at some point post-surgery. Fortunately, pouchitis typically responds well to antibiotic treatment and dietary modifications, allowing most patients to maintain good pouch function.
More serious complications such as pouch failure, strictures, or fistula formation occur in approximately 5-10% of cases. These complications may require additional surgical interventions or, in rare instances, pouch removal. Early recognition and prompt treatment of complications significantly improve the chances of preserving pouch function long-term.
Factors Contributing to Pouch Failure
While J-pouches generally demonstrate excellent durability, certain factors can contribute to pouch failure over time. Chronic pouchitis represents one of the most common causes of long-term problems, potentially leading to scarring and reduced pouch function if left untreated or if it becomes resistant to standard therapies.
Technical surgical factors also influence long-term success. Inadequate blood supply to the pouch, tension on the anastomosis, or improper pouch construction can predispose patients to complications years after the initial surgery. This underscores the importance of having the procedure performed by experienced surgeons at specialized centers.
Patient-related factors such as age, overall health status, and adherence to follow-up care significantly impact long-term outcomes. Younger patients generally experience better long-term function, while older patients may face increased risks of complications. Maintaining regular follow-up appointments and promptly addressing any concerning symptoms helps preserve pouch function over time.
Daily Life with a J-Pouch
Most patients experience significant improvements in their daily bowel function after successful J-pouch surgery and full healing. During the initial recovery period, which typically extends 6-12 months, patients gradually adapt to their new anatomy as the pouch stretches and matures.
Initially, patients may experience 8-12 bowel movements per day, but this frequency typically decreases to 4-8 movements daily as the pouch adapts and expands. Many patients find that their bowel patterns become more predictable over time, allowing them to return to work, travel, and participate in activities they enjoyed before their illness.
Dietary modifications often help optimize pouch function. Many patients benefit from eating smaller, more frequent meals and avoiding certain foods that may cause increased output or gas. Working with a registered dietitian experienced in pouch management can help patients develop sustainable eating patterns that support optimal function.
Long-Term Quality of Life Considerations
Research consistently demonstrates that most patients experience significant improvements in quality of life following successful J-pouch surgery. Studies show that 80-90% of patients report satisfaction with their decision to undergo the procedure, citing improvements in energy levels, social functioning, and overall well-being.
However, patients should maintain realistic expectations about life with a J-pouch. While many return to completely normal activities, some may experience ongoing challenges such as dietary restrictions, occasional urgency, or nighttime bowel movements. These issues typically improve with time and proper management strategies.
Long-term surveillance remains important for J-pouch patients. Regular endoscopic examinations help detect potential complications early, while routine blood work monitors for nutritional deficiencies that may develop over time. Patients who actively participate in their ongoing care typically achieve the best long-term outcomes.
Frequently Asked Questions
How long can a J-pouch last after surgery, and what is the typical lifespan?
Most J-pouches can function effectively for 20-30 years or longer, with studies showing that 85-90% remain functional after 10 years and 80-85% continue working well after 20 years. The actual lifespan varies based on factors such as surgical technique, patient age, underlying condition, and adherence to post-operative care protocols.
What percentage of people have successful J-pouch surgery without complications?
Approximately 90-95% of patients achieve satisfactory functional outcomes following J-pouch surgery. While minor complications like pouchitis may occur in 40-50% of patients, these typically respond well to treatment. Major complications requiring additional surgery occur in only 5-10% of cases.
Can a J-pouch fail years after surgery, and what causes pouch failure?
Yes, J-pouches can fail years after surgery, though this occurs in a minority of cases. Common causes include chronic pouchitis leading to scarring, technical surgical factors such as inadequate blood supply, stricture formation, or fistula development. Patient factors like age and overall health also influence long-term success rates.
How many bowel movements per day should I expect after J-pouch surgery?
Initially, patients may experience 8-12 bowel movements daily, but this typically decreases to 4-8 movements per day as the pouch matures over 6-12 months. The frequency stabilizes as the pouch stretches and adapts, with many patients developing more predictable bowel patterns over time.
What is my quality of life likely to be like living with a J-pouch long-term?
Studies show that 80-90% of J-pouch patients report satisfaction with their decision and significant improvements in quality of life. Most patients return to normal work, travel, and recreational activities. While some may experience ongoing dietary considerations or occasional urgency, the majority enjoy substantially improved energy levels and overall well-being compared to their pre-surgery condition.