Diabetic neuropathy, a serious complication of diabetes that affects the nervous system, raises important questions about life expectancy and quality of life. Understanding how long you can live with neuropathy and what factors influence its progression is crucial for both patients and caregivers. This comprehensive guide explores the timeline of diabetic neuropathy, its impact on longevity, and effective management strategies.
Understanding Life Expectancy with Diabetic Neuropathy
The life expectancy of someone with diabetic neuropathy varies significantly based on several key factors, including blood sugar control, overall health management, and the presence of other complications. While neuropathy itself isn't typically fatal, its complications can significantly impact survival rates and quality of life.
Key Factors Affecting Survival Rates
Several crucial factors influence how long someone can live with diabetic neuropathy:
- Blood glucose management
- Age at diagnosis
- Presence of cardiovascular complications
- Overall diabetes control
- Access to medical care
- Lifestyle factors
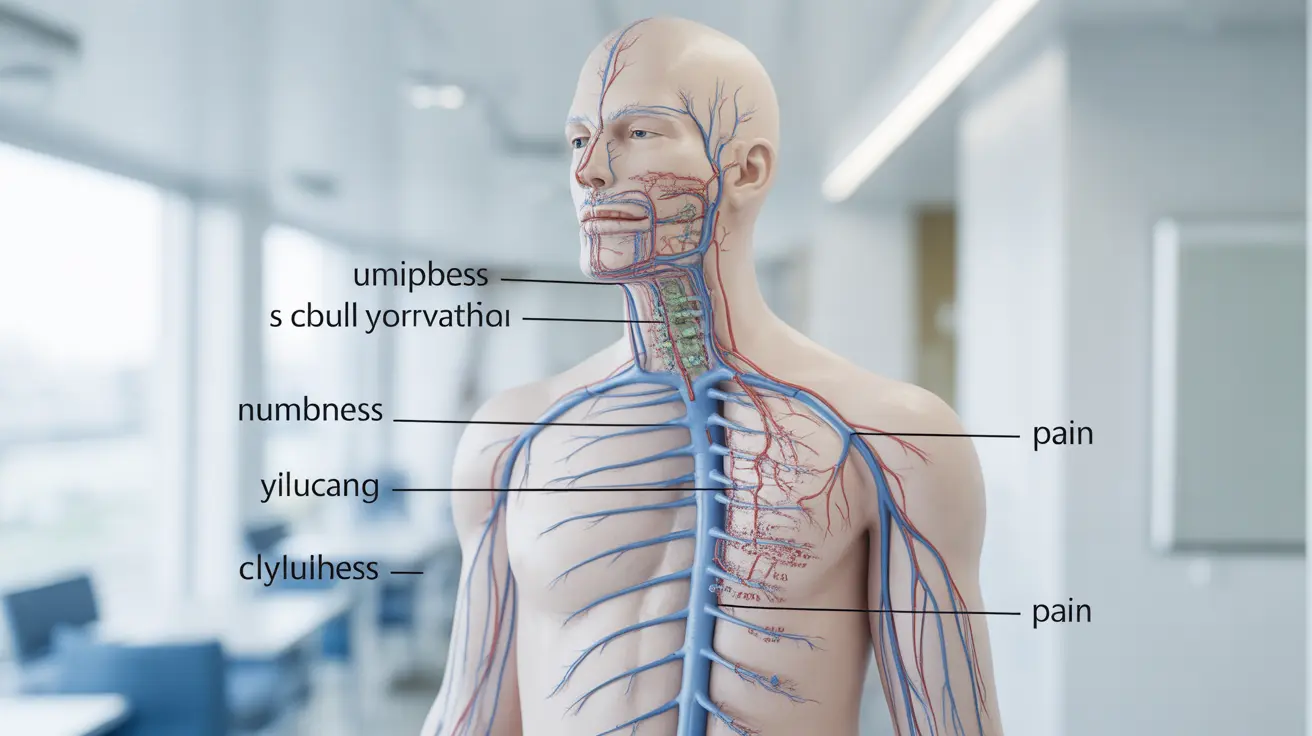
Early Warning Signs and Progression
Recognizing early symptoms is crucial for managing diabetic neuropathy effectively. Initial signs often begin subtly but can progress if left unaddressed:
- Numbness or tingling in feet and hands
- Burning sensations
- Sharp, shooting pains
- Increased sensitivity to touch
- Balance problems
- Muscle weakness
Critical Complications and Risks
Diabetic neuropathy can lead to serious complications that affect life expectancy, particularly when it comes to foot health and infection risk. Understanding these risks is essential for proper management and survival:
- Foot ulcers
- Increased infection risk
- Higher amputation rates
- Cardiovascular complications
- Falls and injuries due to balance issues
Managing and Slowing Progression
Effective management strategies can significantly extend life expectancy and improve quality of life for those with diabetic neuropathy:
Medical Management
- Regular blood sugar monitoring
- Proper medication adherence
- Pain management treatments
- Regular medical check-ups
- Foot care specialists visits
Lifestyle Modifications
Implementing healthy lifestyle changes can help slow progression and improve outcomes:
- Maintaining strict blood sugar control
- Regular physical activity
- Healthy diet
- Smoking cessation
- Regular foot inspections
- Proper footwear
Treatment Options and Recovery Potential
While complete reversal of diabetic neuropathy is rare, various treatments can help manage symptoms and potentially improve nerve function:
- Medications for pain management
- Physical therapy
- Alternative therapies
- Dietary supplements (under medical supervision)
- Advanced wound care when needed
Frequently Asked Questions
How long can someone live with diabetic neuropathy, and what factors influence life expectancy?
Life expectancy with diabetic neuropathy varies greatly depending on blood sugar control, overall health management, and the presence of complications. With proper management and care, many people live for decades after diagnosis. The key factors affecting survival include blood sugar control, cardiovascular health, and how well complications are managed.
What early symptoms indicate the progression of diabetic neuropathy before severe nerve damage occurs?
Early warning signs include tingling or numbness in feet and hands, burning sensations, increased sensitivity to touch, and muscle weakness. Recognizing and addressing these symptoms promptly can help prevent or slow severe nerve damage.
How does diabetic neuropathy affect the risk of foot ulcers and amputations, and what is the impact on survival rates?
Diabetic neuropathy significantly increases the risk of foot ulcers and subsequent amputations due to reduced sensation and poor wound healing. These complications can reduce survival rates, making proper foot care and regular medical monitoring essential.
What are the most effective ways to manage and slow the progression of diabetic neuropathy?
The most effective management strategies include strict blood sugar control, regular exercise, proper nutrition, medication adherence, and regular medical check-ups. Lifestyle modifications and proper foot care are also crucial for slowing progression.
Can diabetic neuropathy be reversed or improved, and what treatments offer the best chances for nerve recovery?
While complete reversal is uncommon, some nerve damage may be improved through strict blood sugar control, appropriate medications, and lifestyle changes. Early intervention and consistent management offer the best chances for potential improvement and symptom control.