Chemotherapy is a crucial treatment for many types of cancer, but it can sometimes affect healthy organs, including the liver. Understanding the relationship between chemotherapy and liver health, as well as the potential for recovery, is essential for patients and healthcare providers alike.
This comprehensive guide explores the impact of chemotherapy on liver function, the possibility of reversal, and important strategies for liver protection during cancer treatment.
How Chemotherapy Affects the Liver
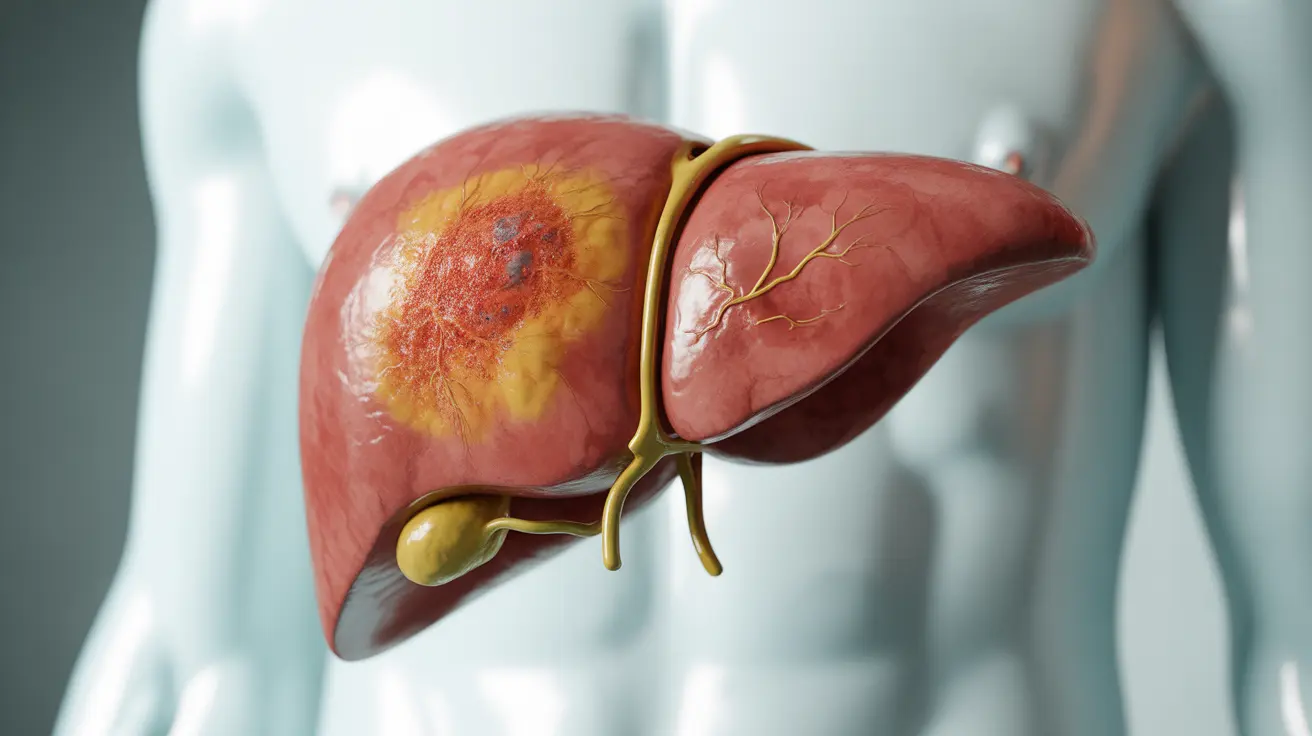
The liver plays a vital role in processing medications, including chemotherapy drugs. During treatment, this important organ can experience various forms of stress and damage:
- Cellular inflammation
- Metabolic changes
- Fatty liver development
- Potential scarring
- Altered enzyme production
The extent and type of liver damage can vary significantly depending on the specific chemotherapy drugs used, treatment duration, and individual patient factors.
Types of Chemotherapy-Related Liver Complications
Chemotherapy can cause several distinct types of liver complications:
Acute Liver Injury
This type of damage typically occurs during or shortly after treatment and may present with elevated liver enzymes, jaundice, or other immediate symptoms.
Chronic Changes
Long-term effects might include:
- Fibrosis
- Fatty liver disease
- Vascular complications
- Portal hypertension
The Potential for Liver Recovery
The liver has remarkable regenerative capabilities, which can support recovery after chemotherapy-induced damage. However, the extent and timeline of recovery depend on several factors:
Factors Affecting Recovery
- The type and duration of chemotherapy
- Pre-existing liver conditions
- Overall health status
- Lifestyle factors
- Genetic predisposition
Many patients experience improvement in liver function after completing chemotherapy, particularly when appropriate supportive measures are implemented.
Protecting Your Liver During Treatment
Several strategies can help minimize liver damage during chemotherapy:
Lifestyle Modifications
- Maintaining a balanced, liver-friendly diet
- Avoiding alcohol completely
- Getting adequate rest
- Staying well-hydrated
- Regular gentle exercise as approved by healthcare providers
Medical Monitoring
Healthcare providers typically monitor liver function through regular blood tests and imaging studies to detect and address any issues early.
Frequently Asked Questions
Can liver damage from chemotherapy be reversed once treatment is completed?
Yes, in many cases, liver damage from chemotherapy can be reversed, especially if it's caught early and proper supportive care is provided. The liver's natural regenerative abilities often enable recovery once chemotherapy is completed, though the timeline varies by individual.
What are the most common types of liver complications caused by chemotherapy?
The most common liver complications from chemotherapy include elevated liver enzymes, fatty liver disease, acute hepatitis, and in some cases, fibrosis. The specific complications depend on the type of chemotherapy drugs used and individual patient factors.
How can you protect your liver from damage during chemotherapy?
You can protect your liver during chemotherapy by following a healthy diet, avoiding alcohol, staying hydrated, taking medications as prescribed, and attending all scheduled monitoring appointments. Regular communication with your healthcare team about any concerns is also crucial.
Is it safe to undergo chemotherapy if you already have cirrhosis or other liver conditions?
While chemotherapy can be administered to patients with pre-existing liver conditions, the treatment plan must be carefully tailored. Dosage adjustments and more frequent monitoring may be necessary, and some chemotherapy agents might need to be avoided.
What are the risk factors that increase the likelihood of liver damage from chemotherapy?
Risk factors include pre-existing liver conditions, alcohol use, certain medications, advanced age, obesity, diabetes, and genetic factors. The specific chemotherapy drugs and cumulative dose also play significant roles in determining risk.