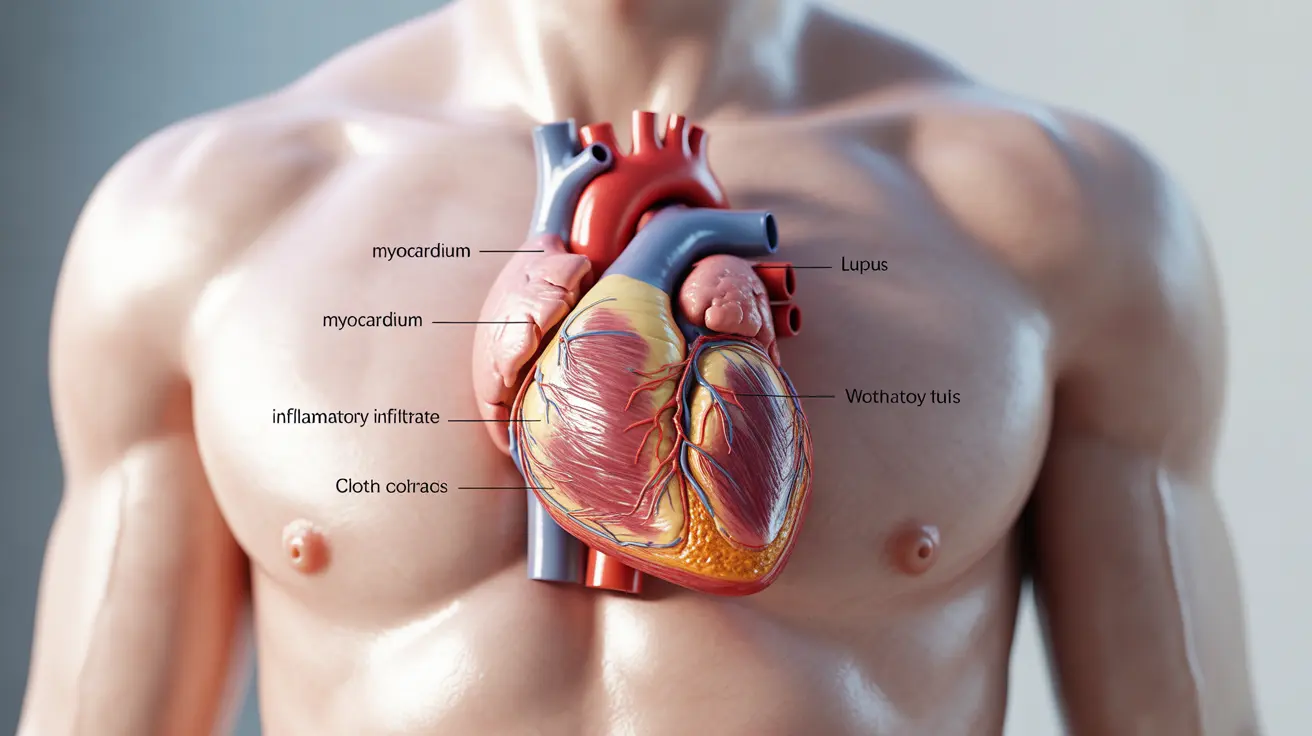
Lupus myocarditis is a serious cardiac complication that can develop in individuals with systemic lupus erythematosus (SLE). This condition occurs when lupus-related inflammation affects the heart muscle, potentially leading to decreased heart function and other cardiovascular complications. Understanding the symptoms, risk factors, and treatment options is crucial for early detection and improved outcomes.
For people living with lupus, recognizing the signs of myocarditis early can make a significant difference in their treatment success and long-term heart health. This comprehensive guide explores the key aspects of lupus myocarditis, from initial symptoms to advanced treatment options.
Key Symptoms of Lupus Myocarditis
Recognizing the symptoms of lupus myocarditis is essential for early intervention. Common signs include:
- Chest pain or discomfort
- Unexplained fatigue
- Shortness of breath, especially during physical activity
- Irregular heartbeat or palpitations
- Rapid or decreased heart rate
- Dizziness or lightheadedness
- Swelling in the legs and ankles
These symptoms may develop gradually or appear suddenly, and their severity can vary significantly among individuals. It's important to note that some patients might experience minimal symptoms initially, making regular medical monitoring crucial for those with lupus.
Diagnostic Approaches and Testing
Diagnosing lupus myocarditis requires a comprehensive evaluation using various diagnostic tools and procedures:
Physical Examination and Medical History
Healthcare providers will conduct a thorough physical examination and review the patient's medical history, particularly focusing on lupus symptoms and cardiac health.
Diagnostic Tests
- Electrocardiogram (ECG)
- Echocardiogram
- Cardiac MRI
- Blood tests for inflammatory markers
- Cardiac enzyme tests
- Chest X-rays
Risk Factors and Prevention
Several factors can increase the likelihood of developing lupus myocarditis:
- Active lupus disease
- History of severe lupus flares
- Presence of other organ involvement
- High levels of inflammatory markers
- Previous cardiac complications
- Delayed lupus diagnosis or treatment
Treatment Strategies
Treatment for lupus myocarditis typically involves a multi-faceted approach:
Immediate Interventions
The primary goal is to reduce inflammation and prevent further heart damage through:
- High-dose corticosteroids
- Immunosuppressive medications
- Careful monitoring of heart function
- Management of fluid retention
Long-term Management
Ongoing care focuses on:
- Regular cardiac monitoring
- Medication adjustment as needed
- Lifestyle modifications
- Stress reduction techniques
- Regular exercise as tolerated
Frequently Asked Questions
What are the most common symptoms of lupus myocarditis to watch out for?
The most common symptoms include chest pain, shortness of breath, fatigue, irregular heartbeat, and swelling in the legs and ankles. Any new or worsening cardiac symptoms should be reported to a healthcare provider immediately.
How is lupus myocarditis diagnosed and what tests are involved?
Diagnosis involves multiple tests including ECG, echocardiogram, cardiac MRI, blood tests, and sometimes cardiac enzyme tests. A comprehensive evaluation helps confirm the diagnosis and assess the extent of heart involvement.
Can lupus myocarditis cause heart failure, and what symptoms indicate this progression?
Yes, lupus myocarditis can lead to heart failure if left untreated. Warning signs include increased shortness of breath, severe fatigue, rapid weight gain, persistent cough, and difficulty breathing when lying flat.
What risk factors increase the likelihood of developing lupus myocarditis?
Key risk factors include active lupus disease, history of severe flares, presence of other organ involvement, high inflammatory markers, and delayed treatment of lupus symptoms.
How is lupus myocarditis treated and what can improve heart function in this condition?
Treatment typically includes high-dose corticosteroids, immunosuppressive medications, and careful monitoring. Improving heart function involves medication compliance, lifestyle modifications, regular monitoring, and following a heart-healthy diet and exercise program as recommended by healthcare providers.