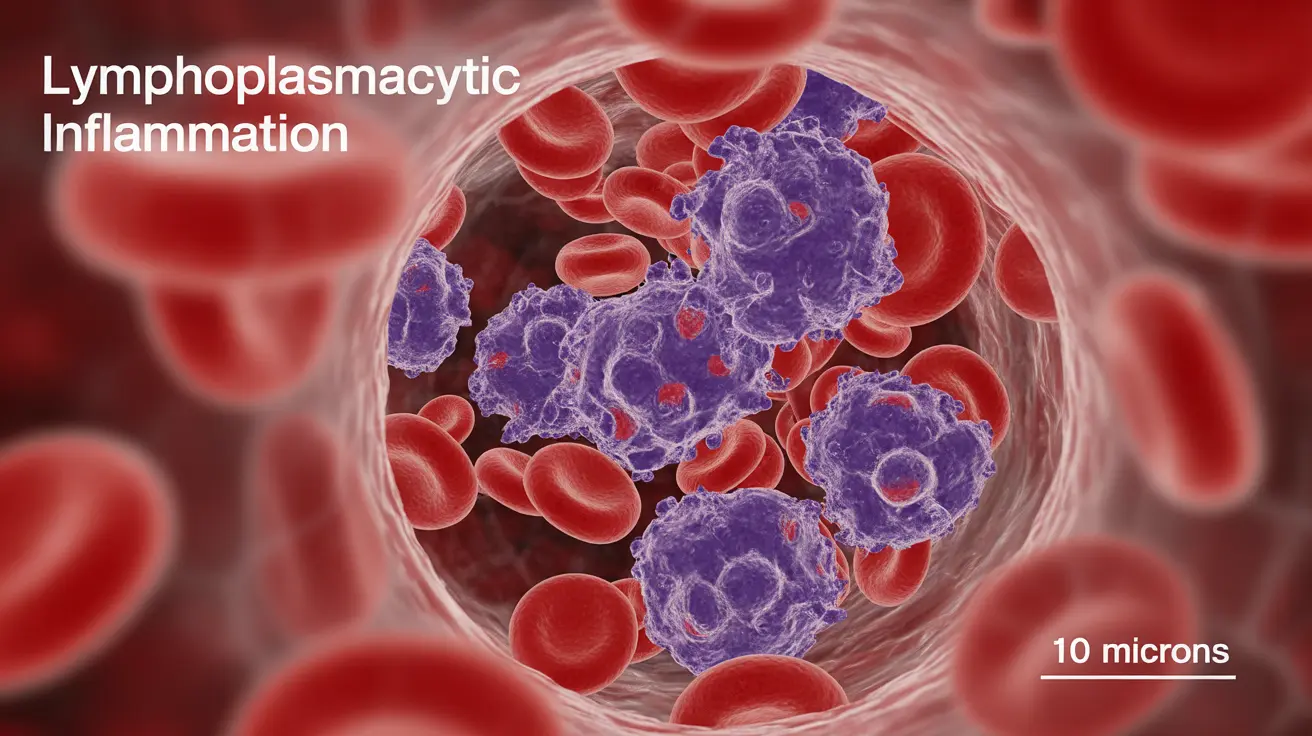
Lymphoplasmacytic inflammation is a complex medical condition that plays a significant role in various blood disorders, particularly in lymphoplasmacytic lymphoma (LPL) and Waldenström macroglobulinemia (WM). This specialized inflammatory process involves specific types of white blood cells and can lead to serious health complications if left unmanaged.
Understanding this condition is crucial for both healthcare providers and patients, as early recognition and proper treatment can significantly impact outcomes. Let's explore the key aspects of lymphoplasmacytic inflammation and its associated disorders in detail.
Signs and Symptoms
The manifestation of lymphoplasmacytic inflammation, particularly in conditions like LPL, can present with various symptoms:
- Unexplained fatigue and weakness
- Frequent infections
- Night sweats
- Unexplained weight loss
- Enlarged lymph nodes
- Easy bruising or bleeding
These symptoms often develop gradually and may be initially subtle, making early detection challenging without proper medical attention.
Diagnostic Approaches
Accurate diagnosis of conditions involving lymphoplasmacytic inflammation requires a comprehensive evaluation:
Blood Tests
Doctors typically begin with complete blood counts and specialized protein tests to identify abnormal antibody levels and assess blood cell populations.
Bone Marrow Examination
A bone marrow biopsy often reveals the presence and extent of lymphoplasmacytic inflammation, helping confirm diagnoses like LPL.
Imaging Studies
CT scans and MRIs may be necessary to evaluate the extent of disease and identify affected areas throughout the body.
Treatment Strategies
Treatment approaches for conditions involving lymphoplasmacytic inflammation vary based on severity and specific diagnosis:
Watch and Wait
Some patients with minimal symptoms may not require immediate treatment but should be monitored regularly for disease progression.
Active Treatment
When treatment becomes necessary, options may include:
- Targeted therapy
- Chemotherapy
- Immunotherapy
- Plasma exchange in cases of severe blood thickness
Managing Complications
Several complications can arise from lymphoplasmacytic inflammation:
Blood Thickness (Hyperviscosity)
This serious condition requires prompt medical attention and may necessitate plasma exchange treatment to prevent circulation problems.
Anemia
Regular monitoring of blood counts and appropriate interventions help manage anemia-related symptoms.
Risk Factors and Prevention
While the exact causes remain unclear, several risk factors have been identified:
- Age (typically affects older adults)
- Family history of blood disorders
- Certain genetic mutations
- Previous exposure to specific chemicals or radiation
Frequently Asked Questions
What are the common symptoms and signs of lymphoplasmacytic lymphoma and Waldenström macroglobulinemia?
Common symptoms include fatigue, night sweats, weight loss, enlarged lymph nodes, and frequent infections. Some patients may experience easy bruising or bleeding due to blood abnormalities.
How is lymphoplasmacytic lymphoma diagnosed and what tests are used to confirm it?
Diagnosis typically involves blood tests, bone marrow biopsy, and imaging studies. Doctors look for specific protein markers and cellular patterns characteristic of the disease.
What treatment options are available for lymphoplasmacytic lymphoma and when is treatment necessary?
Treatment options include targeted therapy, chemotherapy, and immunotherapy. Treatment timing depends on symptom severity and disease progression, with some patients initially managed through careful monitoring.
Can lymphoplasmacytic lymphoma cause complications like anemia or blood thickening, and how are these managed?
Yes, these complications are common. Anemia is managed through regular monitoring and appropriate interventions, while blood thickening may require plasma exchange treatment.
What are the possible causes and risk factors for developing lymphoplasmacytic lymphoma?
Risk factors include advanced age, family history of blood disorders, certain genetic mutations, and environmental exposures. However, the exact causes remain under investigation.