Living with gastroparesis can significantly impact your digestive health, and bloating is a common concern both before diagnosis and after developing this condition. Understanding how bloating manifests in relation to gastroparesis is crucial for managing symptoms and improving quality of life.
This comprehensive guide explores the connection between bloating and gastroparesis, offering practical insights into causes, management strategies, and when to seek medical attention.
What Is Gastroparesis and Its Relationship to Bloating?
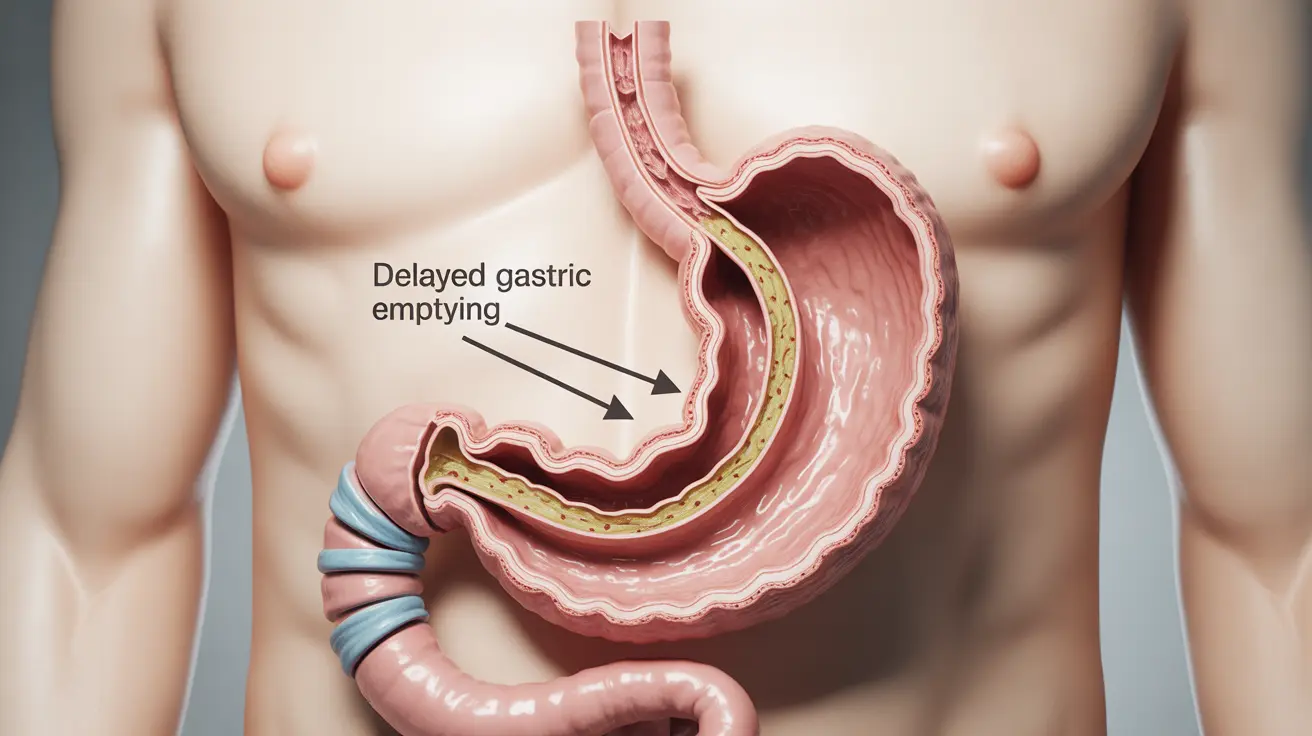
Gastroparesis is a condition where the stomach's ability to empty properly is compromised, leading to delayed gastric emptying. This dysfunction can cause various digestive symptoms, with bloating being particularly troublesome for many patients.
The relationship between bloating and gastroparesis is complex, as bloating can occur both as an early warning sign and as an ongoing symptom after diagnosis.
Understanding Bloating Patterns in Gastroparesis
Early Warning Signs
Before gastroparesis is diagnosed, many patients experience bloating that may seem unexplained or be attributed to other digestive issues. This early bloating often occurs:
- After eating normal-sized meals
- Throughout the day, even with minimal food intake
- Accompanied by early satiety
- Along with occasional nausea
Post-Diagnosis Bloating
Once gastroparesis develops, bloating patterns typically become more predictable and may be:
- More severe after meals
- Longer-lasting than before
- Associated with other gastroparesis symptoms
- More responsive to specific dietary triggers
Managing Bloating with Dietary Modifications
Dietary changes play a crucial role in managing gastroparesis-related bloating. Consider these essential modifications:
- Eat smaller, more frequent meals
- Choose low-fiber, easily digestible foods
- Avoid fatty and high-fiber foods
- Stay well-hydrated throughout the day
- Consume liquids between meals rather than with meals
Medical Interventions for Gastroparesis-Related Bloating
Several medical treatments can help address bloating in gastroparesis patients:
Medications
- Prokinetics to improve stomach emptying
- Anti-nausea medications
- Acid-reducing medications
- Gas-relief medications when appropriate
Other Therapeutic Options
Additional treatments may include:
- Gastric electrical stimulation
- Botox injections in severe cases
- Surgical interventions when conservative treatments fail
When to Seek Medical Care
It's important to consult healthcare providers when experiencing:
- Severe or worsening bloating
- Inability to maintain nutrition
- Significant weight loss
- Persistent vomiting
- Severe abdominal pain
Frequently Asked Questions
What causes bloating before and after gastroparesis develops?
Before gastroparesis develops, bloating may occur due to early stomach emptying problems and nerve dysfunction. After diagnosis, bloating typically results from delayed gastric emptying, bacterial overgrowth, and the stomach's inability to process food properly.
How can I manage or reduce bloating if I have gastroparesis?
Management strategies include eating smaller, frequent meals, avoiding trigger foods, staying upright after eating, gentle exercise when possible, and taking prescribed medications as directed by your healthcare provider.
What dietary changes help prevent bloating in gastroparesis patients?
Key dietary changes include choosing low-fiber foods, avoiding fatty meals, eating smaller portions, thoroughly chewing food, and maintaining proper meal timing. Following a gastroparesis-friendly diet plan can significantly reduce bloating episodes.
Which medications are effective for treating gastroparesis-related bloating?
Effective medications may include prokinetics like metoclopramide, antiemetics for nausea, and sometimes antibiotics for bacterial overgrowth. Your doctor will determine the most appropriate medication based on your specific symptoms and condition severity.
When should I see a doctor for severe bloating or other gastroparesis symptoms?
Seek medical attention if you experience severe or persistent bloating, significant weight loss, inability to keep food down, severe abdominal pain, or if your symptoms significantly impact your quality of life despite following management strategies.