Hemorrhoids after pregnancy are an incredibly common condition that affects up to 50% of women who have recently given birth. These swollen, inflamed blood vessels in the rectal and anal area can cause significant discomfort during what should be a joyful recovery period. While hemorrhoids can develop during pregnancy due to increased pressure from the growing uterus, they often become more pronounced or first appear after delivery, particularly following vaginal birth.
Understanding how to recognize, treat, and manage postpartum hemorrhoids is essential for new mothers seeking relief and a smoother recovery. With proper care and attention, most women can effectively manage their symptoms and return to comfortable daily activities within weeks of delivery.
Understanding the Causes of Postpartum Hemorrhoids
Several factors contribute to the development of hemorrhoids after pregnancy and vaginal delivery. The birthing process places tremendous pressure on the pelvic floor muscles and blood vessels in the anal and rectal area. During the pushing stage of labor, intense straining can cause existing hemorrhoids to worsen or new ones to form as blood vessels become engorged and inflamed.
Pregnancy itself creates conditions that predispose women to hemorrhoid development. The growing uterus puts increasing pressure on the pelvic blood vessels, particularly the inferior vena cava, which can impede blood flow and cause vessels to swell. Additionally, pregnancy hormones like progesterone relax blood vessel walls, making them more susceptible to stretching and inflammation.
Constipation, which commonly affects pregnant and postpartum women due to hormonal changes, iron supplements, and reduced physical activity, further contributes to hemorrhoid formation. Straining during bowel movements increases pressure on anal blood vessels, leading to swelling and irritation that can persist well after delivery.
Recognizing Symptoms of Postpartum Hemorrhoids
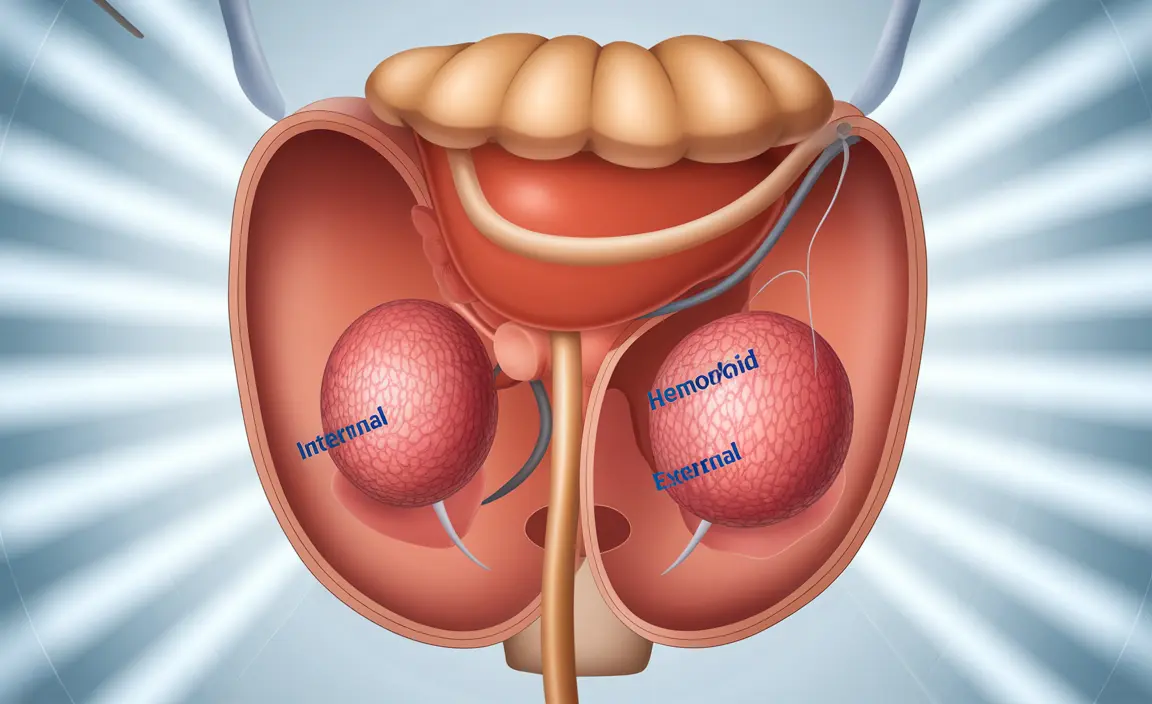
Postpartum hemorrhoids can manifest in various ways, and symptoms may differ depending on whether they are internal or external. External hemorrhoids, located around the anal opening, are typically more painful and noticeable, while internal hemorrhoids develop inside the rectum and may cause less obvious discomfort initially.
Common symptoms include persistent pain, itching, or burning sensations around the anal area that may worsen during bowel movements or when sitting for extended periods. Many women notice bright red blood on toilet paper or in the toilet bowl, which can be alarming but is typically not dangerous unless bleeding becomes excessive.
Swelling and inflammation around the anus are frequent indicators, sometimes accompanied by the sensation of incomplete bowel evacuation. Some women may feel or see small, grape-like lumps around the anal opening, particularly with external hemorrhoids. Discomfort often intensifies when sitting, making activities like nursing or resting challenging during early recovery.
Duration and Natural Healing Process
The duration of hemorrhoids after pregnancy varies significantly among individuals, typically lasting anywhere from a few weeks to several months. Most mild to moderate hemorrhoids begin improving within the first few weeks postpartum as pressure on pelvic blood vessels decreases and hormonal changes stabilize.
For many women, hemorrhoids do resolve naturally without medical intervention, particularly when combined with appropriate self-care measures. The body's natural healing processes work to reduce inflammation and restore normal blood flow to affected areas as recovery progresses. However, the timeline depends on various factors including hemorrhoid severity, individual healing capacity, and adherence to recommended lifestyle modifications.
Factors that may prolong healing include continued constipation, lack of physical activity, poor dietary habits, or underlying conditions that affect circulation. Women who experience severe hemorrhoids or those with complications may require longer recovery periods and potentially medical intervention to achieve complete resolution.
Effective Home Treatments and Self-Care Strategies
Several home remedies and lifestyle adjustments can significantly improve hemorrhoid symptoms and accelerate healing. Warm sitz baths, taken 2-3 times daily for 10-15 minutes, help reduce inflammation, improve circulation, and provide immediate pain relief. Adding Epsom salts to the bathwater may enhance the soothing effects.
Dietary modifications play a crucial role in managing postpartum hemorrhoids. Increasing fiber intake through fruits, vegetables, whole grains, and legumes helps soften stools and reduce straining during bowel movements. Adequate hydration, aiming for 8-10 glasses of water daily, supports proper digestion and prevents constipation.
Cold therapy using ice packs or cold compresses applied for 10-15 minutes several times daily can help reduce swelling and numb pain. Alternating between warm baths and cold applications often provides optimal relief. Over-the-counter treatments like witch hazel pads, hemorrhoid creams containing hydrocortisone, or topical anesthetics can offer additional symptom management.
Establishing regular, gentle exercise routines as soon as medically approved helps improve circulation and prevent constipation. Simple activities like walking, pelvic floor exercises, and gentle stretching can be beneficial. Avoiding prolonged sitting or standing, using a donut cushion when necessary, and maintaining proper toilet habits also support healing.
When to Seek Medical Attention
While most postpartum hemorrhoids can be managed at home, certain situations warrant professional medical evaluation. Excessive bleeding that soaks pads or persists beyond normal spotting requires immediate attention, as it may indicate complications or other underlying conditions.
Severe pain that doesn't respond to conservative treatments, signs of infection such as fever or pus discharge, or hemorrhoids that don't improve after 4-6 weeks of consistent home treatment should prompt a healthcare visit. Additionally, if hemorrhoids significantly interfere with daily activities, breastfeeding, or bonding with the baby, professional guidance can help identify more effective treatment options.
Medical treatments for persistent hemorrhoids may include prescription-strength topical medications, minimally invasive procedures like rubber band ligation or sclerotherapy, or in severe cases, surgical removal. Healthcare providers can also rule out other conditions that may mimic hemorrhoid symptoms and provide personalized treatment recommendations based on individual circumstances.
Frequently Asked Questions
What causes hemorrhoids to develop after pregnancy and vaginal delivery?
Hemorrhoids develop after pregnancy primarily due to the intense pressure placed on pelvic blood vessels during labor and delivery. The pushing stage of vaginal birth causes significant straining that can enlarge existing hemorrhoids or create new ones. Additionally, pregnancy hormones soften blood vessel walls, making them more prone to swelling, while the growing uterus throughout pregnancy puts continuous pressure on pelvic circulation, setting the stage for postpartum hemorrhoid development.
What are the common symptoms of postpartum hemorrhoids to watch for?
Common symptoms include pain, itching, or burning sensations around the anal area, especially during bowel movements. Many women notice bright red blood on toilet paper or in the toilet bowl, along with swelling or small lumps around the anus. Other signs include discomfort when sitting, a feeling of incomplete bowel evacuation, and general irritation in the rectal area that may worsen throughout the day or with certain activities.
How long do hemorrhoids typically last after giving birth, and will they go away on their own?
Postpartum hemorrhoids typically last from a few weeks to several months, with most mild cases improving within 4-6 weeks after delivery. Many hemorrhoids do resolve naturally as hormonal changes stabilize and pressure on pelvic blood vessels decreases. However, the healing timeline depends on factors like hemorrhoid severity, individual healing capacity, and whether proper self-care measures are followed. Severe cases may require medical intervention for complete resolution.
What home treatments and lifestyle changes can help relieve hemorrhoids after pregnancy?
Effective home treatments include warm sitz baths 2-3 times daily, increasing dietary fiber intake, staying well-hydrated, and applying cold compresses to reduce swelling. Over-the-counter treatments like witch hazel pads and hemorrhoid creams can provide additional relief. Lifestyle changes such as avoiding prolonged sitting, establishing regular gentle exercise routines, preventing constipation through proper diet, and using proper toilet habits all support healing and symptom management.
When should I see a doctor about postpartum hemorrhoids, and what medical treatments might be necessary?
Seek medical attention if you experience excessive bleeding, severe pain unresponsive to home treatments, signs of infection like fever or pus, or if hemorrhoids don't improve after 4-6 weeks of consistent self-care. Medical treatments may include prescription-strength topical medications, minimally invasive procedures like rubber band ligation or sclerotherapy, or in severe cases, surgical removal. Healthcare providers can also evaluate for other conditions and provide personalized treatment recommendations based on your specific situation.