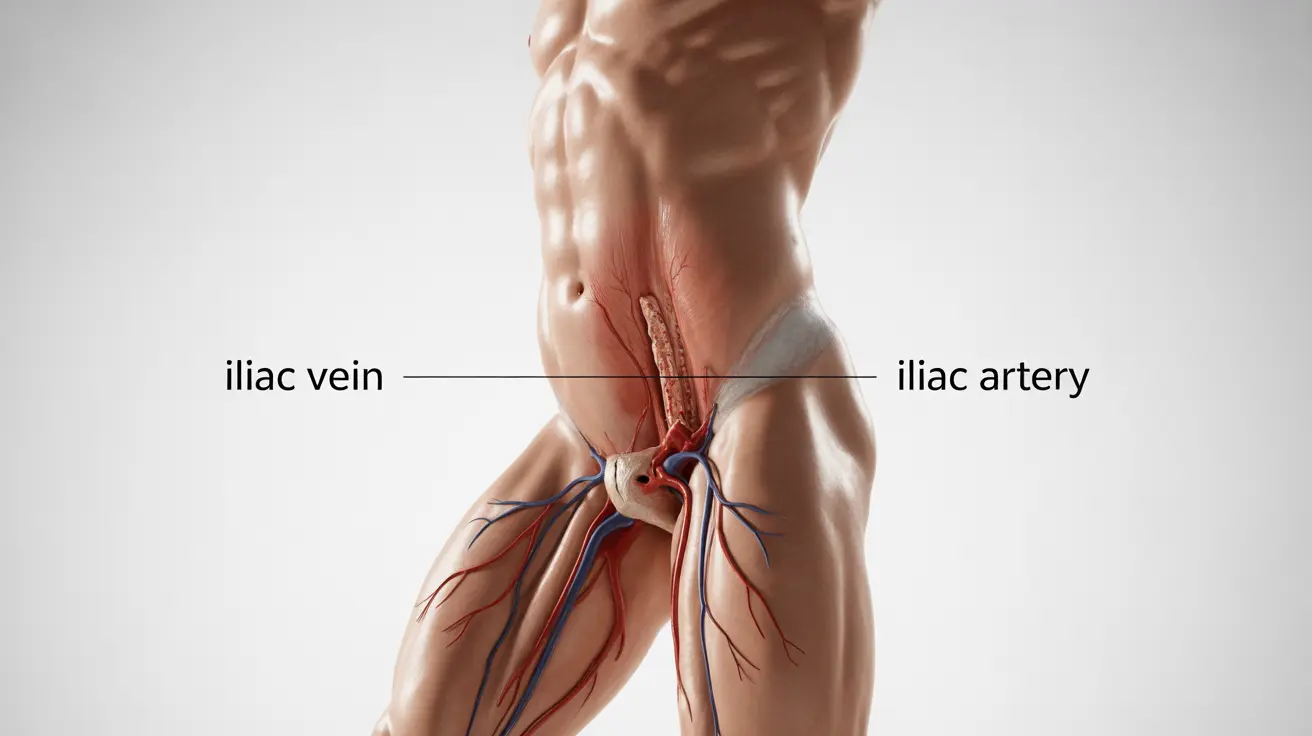
May-Thurner syndrome (MTS) is a rare but potentially serious vascular condition where the left iliac vein becomes compressed by the right iliac artery against the spine. This compression can lead to dangerous blood clots and requires careful medical attention to prevent life-threatening complications.
Understanding the risks and recognizing the symptoms of May-Thurner syndrome is crucial for early intervention and successful treatment. This comprehensive guide explores the warning signs, diagnostic approaches, and available treatments to help you better understand this condition.
Key Signs and Symptoms to Watch For
May-Thurner syndrome often presents with distinctive symptoms, particularly in the left leg. Common indicators include:
- Swelling in the left leg
- Pain or tenderness in the affected leg
- Skin discoloration or warmth
- Visible surface veins
- Heaviness or fatigue in the leg
- Ulcers that are slow to heal
These symptoms typically develop gradually and may worsen with prolonged standing or physical activity. It's essential to seek medical attention if you experience persistent leg swelling or pain, especially if it's predominantly on the left side.
Understanding the Serious Complications
May-Thurner syndrome can lead to severe complications if left untreated. The most significant risks include:
- Deep Vein Thrombosis (DVT)
- Pulmonary Embolism
- Chronic Venous Insufficiency
- Post-thrombotic Syndrome
The compression of the iliac vein can create ideal conditions for blood clot formation. These clots may break loose and travel to the lungs, causing a potentially fatal pulmonary embolism. Early intervention is crucial for preventing these life-threatening complications.
Diagnostic Process and Testing
Diagnosing May-Thurner syndrome requires several specialized imaging tests and procedures:
- Venous Ultrasound
- CT Venography
- MR Venography
- Intravascular Ultrasound (IVUS)
- Venography
Healthcare providers typically begin with non-invasive tests before proceeding to more detailed imaging studies. The goal is to confirm the presence of venous compression and assess any existing blood clots.
Treatment Approaches
Treatment for May-Thurner syndrome focuses on improving blood flow and preventing clot formation. Options include:
Conservative Management
- Compression stockings
- Regular exercise
- Elevation of legs
- Blood-thinning medications
Interventional Procedures
- Angioplasty and stenting
- Catheter-directed thrombolysis
- Surgical bypass (in severe cases)
The choice of treatment depends on the severity of symptoms, presence of blood clots, and overall health status of the patient.
Frequently Asked Questions
What are the signs and symptoms of May-Thurner syndrome I should watch for?
Key symptoms include left leg swelling, pain, skin changes, and visible surface veins. Watch for persistent discomfort or swelling that worsens with activity or standing.
Can May-Thurner syndrome cause death, and how does it lead to serious complications like pulmonary embolism?
Yes, May-Thurner syndrome can be life-threatening if untreated. The main risk comes from blood clots (DVT) that can break loose and travel to the lungs, causing a potentially fatal pulmonary embolism.
How is May-Thurner syndrome diagnosed and what tests are used to detect it?
Diagnosis typically involves imaging tests such as venous ultrasound, CT venography, MR venography, and sometimes intravascular ultrasound. These tests help visualize the vein compression and identify any existing blood clots.
What treatment options are available to prevent blood clots and other risks associated with May-Thurner syndrome?
Treatment options range from conservative measures like compression stockings and blood thinners to interventional procedures such as angioplasty and stenting. The specific approach depends on individual patient factors and severity of the condition.
How can I reduce my risk of developing complications if I have May-Thurner syndrome?
Risk reduction strategies include regular physical activity, wearing prescribed compression stockings, taking prescribed medications as directed, maintaining a healthy weight, and avoiding prolonged periods of immobility. Regular follow-up with healthcare providers is also essential.