Living with arthritis can be challenging, and understanding your Medicare coverage options is crucial for managing treatment costs effectively. This comprehensive guide explores how Medicare covers various arthritis treatments, from medications to surgery, helping you navigate your healthcare benefits with confidence.
Whether you're dealing with osteoarthritis, rheumatoid arthritis, or other forms of joint disease, knowing what Medicare covers can help you make informed decisions about your treatment plan while managing out-of-pocket expenses.
Medicare Coverage for Arthritis Medications
Medicare provides coverage for various arthritis medications through different parts of its program. Part D prescription drug plans typically cover many common arthritis medications, including:
- NSAIDs (nonsteroidal anti-inflammatory drugs)
- Corticosteroids
- Disease-modifying antirheumatic drugs (DMARDs)
- Biologic medications
Coverage levels and costs vary depending on your specific plan and the medication's tier placement in your plan's formulary. Some specialty medications, particularly biologics, may require prior authorization or step therapy.
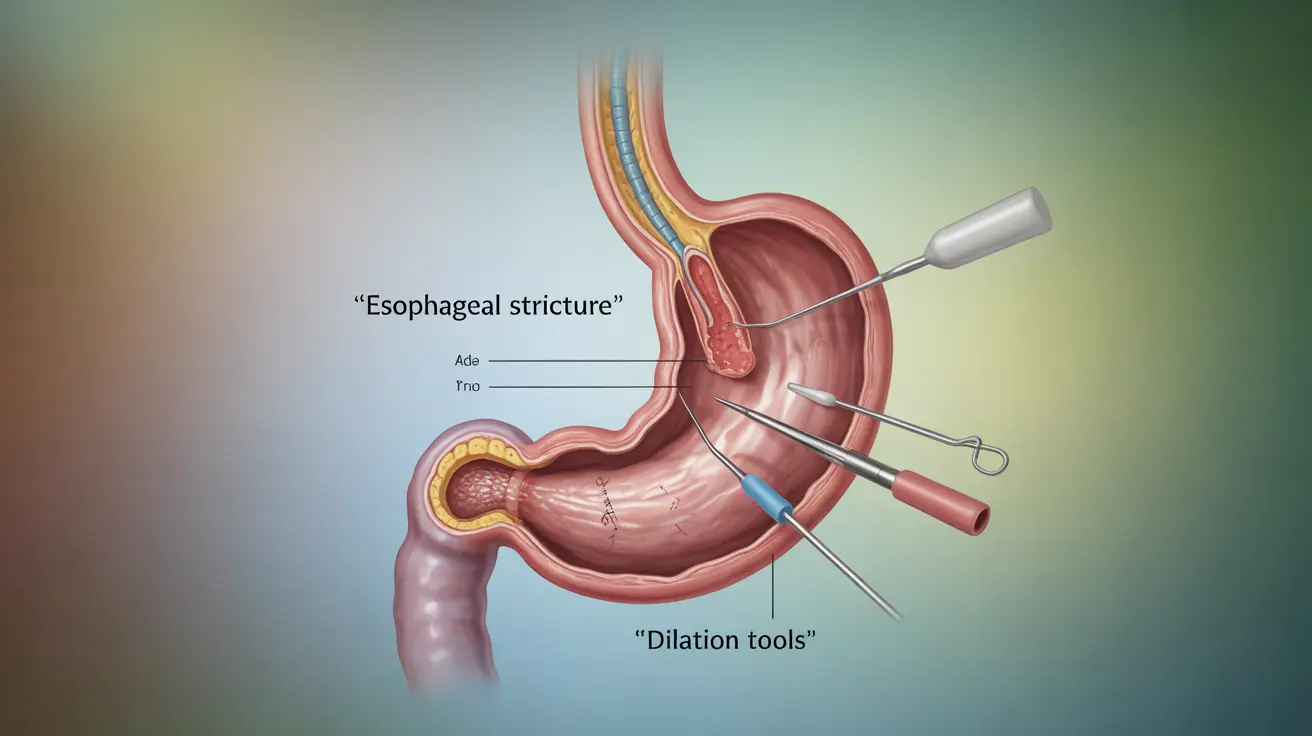
Surgical Procedures and Hospital Coverage
Medicare Part A covers inpatient hospital stays for arthritis-related surgeries, while Part B covers outpatient procedures. Common covered procedures include:
- Joint replacement surgery
- Arthroscopic procedures
- Synovectomy
- Joint fusion operations
To qualify for coverage, procedures must be deemed medically necessary by your healthcare provider and approved by Medicare. You'll need to meet your deductible and pay applicable coinsurance.
Physical Therapy and Medical Equipment
Medicare Part B covers medically necessary physical therapy services for arthritis patients. This includes:
- Individual therapy sessions
- Exercise programs
- Pain management techniques
- Mobility training
Additionally, Medicare covers durable medical equipment (DME) when prescribed by your doctor:
- Walkers and canes
- Braces and supports
- Wheelchair or mobility scooters
- Other assistive devices
Alternative Treatments and Supplementary Care
Medicare has expanded its coverage to include some alternative treatments for arthritis management:
- Acupuncture (limited coverage for chronic lower back pain)
- Chiropractic care (limited to manual manipulation of the spine)
- Occupational therapy
- Therapeutic exercises
Coverage for these services may have specific requirements and limitations, so it's important to verify coverage before beginning treatment.
Frequently Asked Questions
Does Medicare cover arthritis medications, including biologics and DMARDs?
Yes, Medicare Part D covers many arthritis medications, including biologics and DMARDs. Coverage levels vary by plan, and some medications may require prior authorization. Part B may cover certain medications administered in a medical setting.
What types of arthritis surgery does Medicare insurance pay for, and what are the requirements?
Medicare covers medically necessary surgeries like joint replacements, arthroscopic procedures, and joint fusions. The procedures must be ordered by a Medicare-approved physician and meet medical necessity criteria. Part A covers inpatient procedures, while Part B covers outpatient surgeries.
What out-of-pocket costs should I expect for arthritis treatment with Medicare?
Out-of-pocket costs include deductibles, copayments, and coinsurance. For 2024, the Part A deductible applies to hospital stays, while Part B requires a separate deductible and typically 20% coinsurance for covered services. Part D medication costs vary by plan and drug tier.
Is physical therapy or medical equipment like braces covered by Medicare for arthritis?
Yes, Medicare Part B covers medically necessary physical therapy and durable medical equipment like braces when prescribed by your doctor. You'll typically pay 20% of the Medicare-approved amount after meeting your deductible.
Are alternative treatments such as acupuncture for arthritis covered by Medicare?
Medicare offers limited coverage for some alternative treatments. Acupuncture is covered specifically for chronic lower back pain, while chiropractic care is covered only for spinal manipulation. Coverage for other alternative treatments varies and may require specific medical necessity documentation.