Temporomandibular joint (TMJ) disorders affect millions of Americans, causing jaw pain, difficulty chewing, and other debilitating symptoms. For Medicare beneficiaries dealing with TMJ issues, understanding what treatments are covered can be challenging and confusing. The reality is that Medicare coverage for TMJ treatment is limited and often depends on specific circumstances and the type of care needed.
Navigating Medicare's coverage policies for TMJ treatment requires understanding the distinction between medical and dental care, as well as knowing which specific situations may qualify for coverage. This comprehensive guide will help you understand when Medicare does and doesn't cover TMJ treatments, what alternatives may be available, and how to maximize your benefits.
Understanding TMJ Disorders and Treatment Options
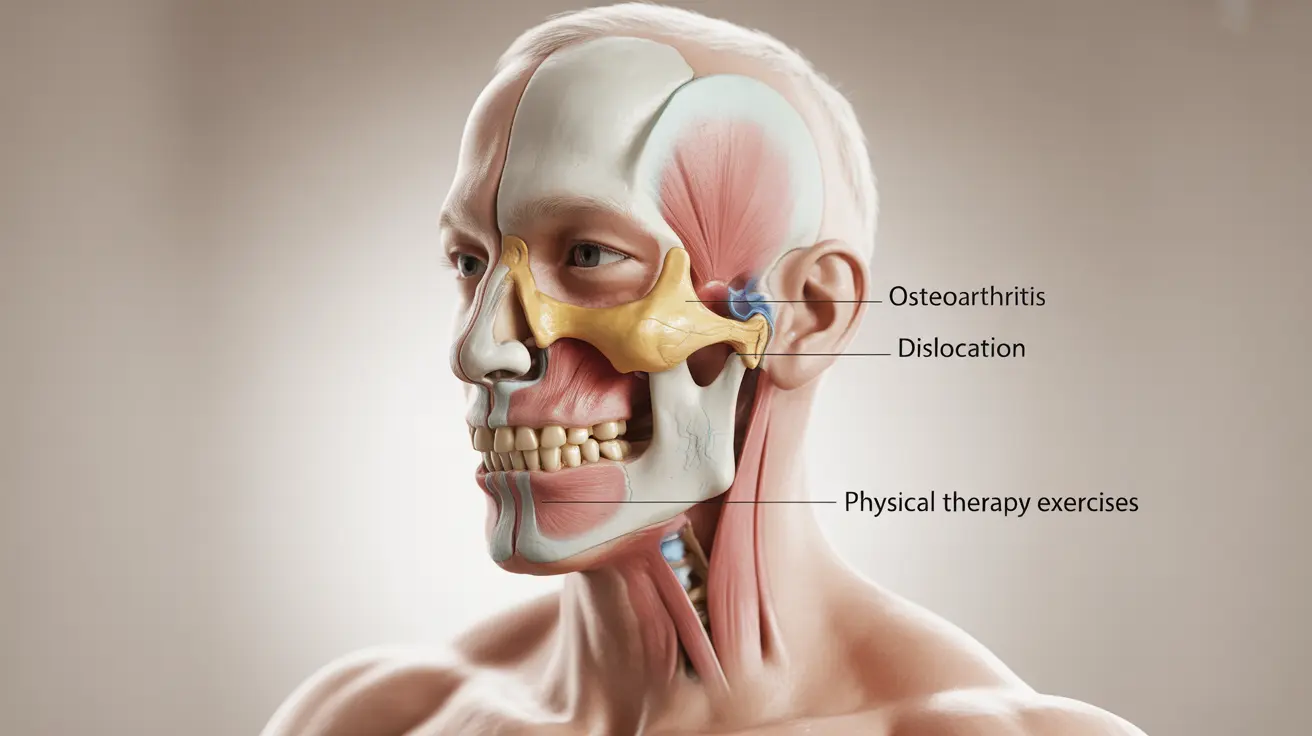
TMJ disorders encompass a range of conditions affecting the temporomandibular joint, which connects your jawbone to your skull. These disorders can result from various factors, including arthritis, jaw injury, muscle tension, or teeth grinding. Common symptoms include jaw pain, clicking or popping sounds when opening the mouth, difficulty chewing, and facial pain.
Treatment approaches for TMJ disorders vary widely, ranging from conservative methods like physical therapy and lifestyle modifications to more intensive interventions such as oral appliances, injections, or surgical procedures. The type of treatment recommended often depends on the severity of symptoms and the underlying cause of the disorder.
Medicare Coverage for TMJ Surgery
Medicare Part A may cover TMJ surgery in very specific circumstances, but the bar for approval is quite high. For surgical treatment to be covered, the procedure must be considered medically necessary rather than dental in nature. This typically means the TMJ disorder must be causing significant functional impairment that affects your ability to eat, speak, or perform daily activities.
Medically necessary TMJ surgery under Medicare usually involves cases where there is clear structural damage to the joint, severe arthritis, or other conditions that require hospital-based surgical intervention. The surgery must be performed in a hospital or ambulatory surgical center, and extensive documentation is required to demonstrate medical necessity.
However, it's important to note that Medicare approval for TMJ surgery is rare. Most TMJ-related procedures are considered dental rather than medical, which places them outside of traditional Medicare coverage. Prior authorization is typically required, and beneficiaries should expect thorough review of their case before any approval is granted.
Physical Therapy Coverage Under Medicare Part B
Medicare Part B does provide coverage for physical therapy when it's prescribed by a physician and deemed medically necessary for treating TMJ disorders. This represents one of the more accessible treatment options for Medicare beneficiaries with TMJ issues.
Covered physical therapy services may include exercises to improve jaw mobility, techniques to reduce muscle tension, and education about proper jaw positioning. The therapy must be provided by a licensed physical therapist or other qualified healthcare professional, and it must follow a physician-prescribed treatment plan.
To qualify for coverage, the physical therapy must show measurable improvement in your condition and functional abilities. Medicare typically covers a limited number of sessions per year, and beneficiaries are responsible for the standard Part B coinsurance of 20% after meeting their annual deductible.
Dental Appliances and Medicare Coverage Limitations
Unfortunately, Medicare generally does not cover dental appliances used to treat TMJ disorders, including mouthguards, splints, or bite guards. These devices are typically classified as dental equipment rather than durable medical equipment, placing them outside Medicare's standard coverage parameters.
This exclusion applies even when these appliances are prescribed by a physician rather than a dentist and are intended to treat medical symptoms like jaw pain or headaches. The distinction between medical and dental care is strictly maintained in Medicare's coverage policies, often to the disadvantage of beneficiaries with TMJ disorders.
Some exceptions may exist in cases where the appliance is directly related to covered medical treatment, such as following jaw surgery. However, these exceptions are rare and require extensive documentation and prior authorization.
Prescription Drug Coverage for TMJ
Medicare Part D plans and Medicare Advantage plans with prescription drug coverage may help cover medications used to treat TMJ-related symptoms. This can include pain relievers, muscle relaxants, anti-inflammatory drugs, and other medications prescribed specifically for TMJ management.
Coverage varies significantly between different Part D plans, so it's essential to review your plan's formulary to understand which TMJ-related medications are covered and at what cost. Some medications may require prior authorization or step therapy, where you must try less expensive alternatives first.
Medicare Advantage plans may offer additional prescription drug benefits beyond standard Part D coverage, potentially including better access to specialized TMJ medications or lower copayments for frequently prescribed treatments.
Why Original Medicare Excludes Most TMJ Treatments
The primary reason Original Medicare (Parts A and B) excludes most TMJ treatments stems from the historical classification of TMJ disorders as primarily dental rather than medical conditions. When Medicare was established, clear distinctions were made between medical and dental care, with dental services largely excluded from coverage.
This classification persists today, despite growing recognition that TMJ disorders can have significant medical implications beyond dental health. The jaw joint's complexity and its relationship to broader musculoskeletal and neurological systems make this distinction increasingly problematic for patients seeking comprehensive care.
Additionally, Medicare's focus on acute care rather than chronic condition management contributes to limited TMJ coverage. Many TMJ treatments are considered ongoing maintenance rather than curative medical interventions, which aligns less favorably with Medicare's traditional coverage philosophy.
Alternative Coverage Options
Medicare beneficiaries with TMJ disorders may find better coverage through Medicare Advantage plans, which sometimes include dental benefits that could extend to TMJ-related appliances or treatments. These plans vary widely in their offerings, so careful comparison shopping is essential.
Supplemental insurance policies, including dental insurance or specific TMJ coverage plans, may help bridge the gap left by Medicare's limited coverage. Some employers offer retiree health benefits that include more comprehensive TMJ treatment coverage.
Frequently Asked Questions
Does Medicare cover TMJ surgery and under what conditions is it considered medically necessary?
Medicare Part A may cover TMJ surgery only when it's deemed medically necessary, which typically requires clear structural joint damage, severe arthritis, or significant functional impairment affecting eating, speaking, or daily activities. The surgery must be performed in a hospital setting, and extensive documentation proving medical rather than dental necessity is required. However, approval is rare, as most TMJ procedures are classified as dental care.
Can Medicare Part B pay for physical therapy to treat TMJ disorders?
Yes, Medicare Part B covers physical therapy for TMJ disorders when prescribed by a physician and considered medically necessary. Covered services include jaw mobility exercises, muscle tension reduction techniques, and proper jaw positioning education. The therapy must be provided by licensed professionals following a physician's treatment plan and show measurable functional improvement. Beneficiaries pay 20% coinsurance after meeting their annual deductible.
Are dental appliances like mouthguards or splints for TMJ covered by Medicare?
No, Medicare generally does not cover dental appliances for TMJ treatment, including mouthguards, splints, or bite guards. These devices are classified as dental equipment rather than durable medical equipment, placing them outside Medicare's coverage scope. This exclusion applies even when prescribed by physicians for medical symptoms. Rare exceptions may exist following covered jaw surgery, but these require extensive documentation and prior authorization.
How does Medicare Part D or Medicare Advantage cover prescription medications for TMJ?
Medicare Part D plans and Medicare Advantage plans with prescription coverage may help pay for TMJ-related medications, including pain relievers, muscle relaxants, and anti-inflammatory drugs. Coverage varies significantly between plans, so reviewing your plan's formulary is essential. Some medications may require prior authorization or step therapy. Medicare Advantage plans may offer enhanced prescription benefits with better access to specialized TMJ medications or lower copayments.
Why does Original Medicare (Parts A and B) usually exclude most TMJ treatments from coverage?
Original Medicare excludes most TMJ treatments because these disorders are historically classified as dental rather than medical conditions. This classification dates back to Medicare's establishment when clear distinctions were made between medical and dental care. Additionally, Medicare's focus on acute care rather than chronic condition management contributes to limited coverage, as many TMJ treatments are considered ongoing maintenance rather than curative medical interventions.