Meloxicam, a commonly prescribed nonsteroidal anti-inflammatory drug (NSAID), effectively manages conditions like arthritis and acute pain. However, many patients and healthcare providers have questions about its potential effects on liver health. Understanding these impacts is crucial for safe and effective treatment.
While meloxicam is generally considered safe when taken as prescribed, it's important to be aware of its potential effects on liver function and know how to recognize warning signs of liver-related complications.
How Meloxicam Affects the Liver
The liver plays a crucial role in processing medications, including meloxicam. Like other NSAIDs, meloxicam undergoes metabolization in the liver, where it's broken down and prepared for elimination from the body. While most people tolerate this process well, some individuals may experience liver-related side effects.
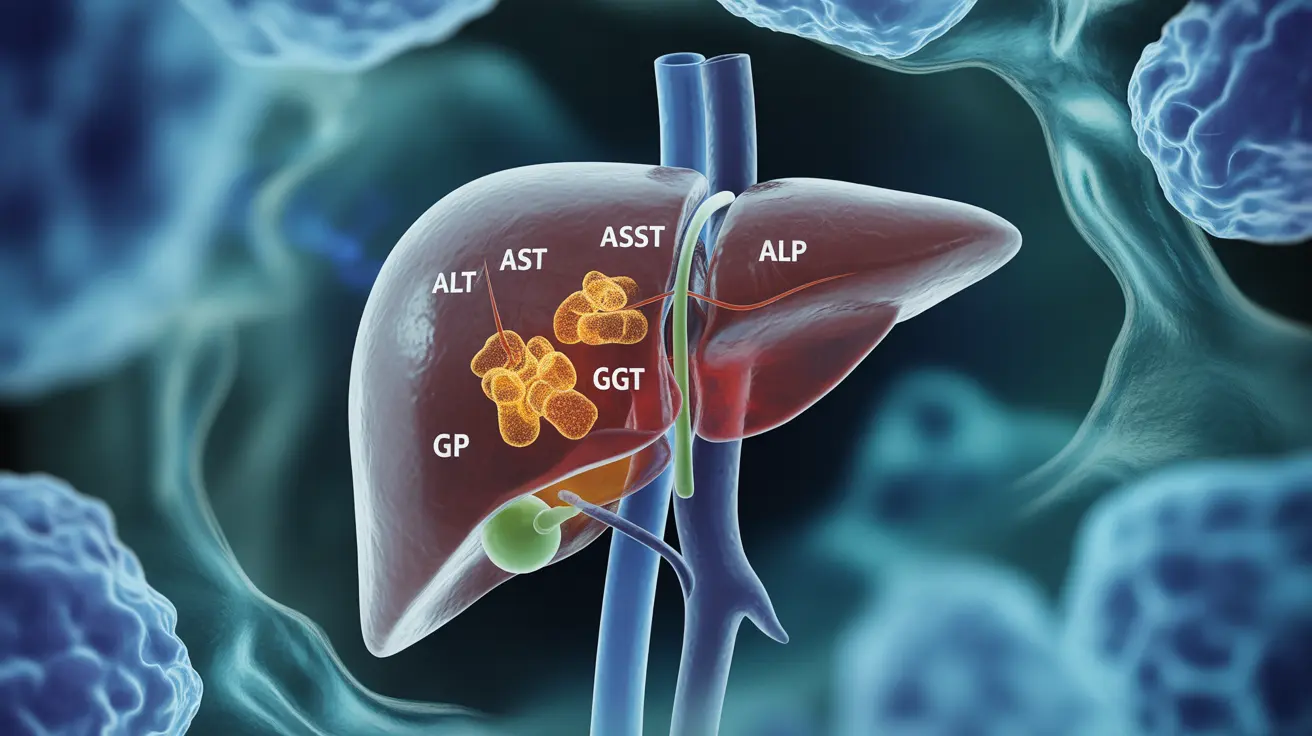
Understanding Liver Function Tests
Healthcare providers often monitor liver function through blood tests that measure various enzyme levels, including:
- Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Alkaline phosphatase (ALP)
- Gamma-glutamyl transferase (GGT)
Signs of Liver Problems During Meloxicam Use
Recognizing potential liver-related complications early is essential. Watch for these warning signs:
- Yellowing of the skin or eyes (jaundice)
- Unusual fatigue or weakness
- Dark urine
- Light-colored stools
- Upper right abdominal pain
- Unexplained nausea or vomiting
- Loss of appetite
Risk Factors and Prevention
Certain factors may increase the risk of liver-related complications while taking meloxicam:
- Pre-existing liver conditions
- Heavy alcohol consumption
- Advanced age
- Use of other medications that affect the liver
- History of liver reactions to medications
Preventive Measures
To minimize the risk of liver problems while taking meloxicam:
- Follow prescribed dosage strictly
- Avoid alcohol or limit consumption
- Inform your healthcare provider about all medications and supplements
- Attend regular check-ups and monitoring appointments
- Report any concerning symptoms promptly
Monitoring Requirements
Regular monitoring of liver function may be necessary for some patients taking meloxicam, particularly those with risk factors or long-term use. Your healthcare provider will determine the appropriate frequency of monitoring based on your individual circumstances.
Frequently Asked Questions
Can meloxicam cause liver damage or affect liver function?
Yes, meloxicam can potentially affect liver function, though serious liver damage is relatively rare. Like other NSAIDs, it may cause elevated liver enzymes in some individuals, particularly with long-term use or in those with risk factors.
What symptoms indicate liver problems when taking meloxicam?
Key symptoms include yellowing of the skin or eyes (jaundice), unusual fatigue, dark urine, light-colored stools, upper right abdominal pain, nausea, and loss of appetite. If you experience any of these symptoms, contact your healthcare provider immediately.
How common are elevated liver enzymes in people using meloxicam?
Elevated liver enzymes occur in a small percentage of meloxicam users, typically less than 5%. Most cases are mild and resolve with dose adjustment or discontinuation of the medication.
Should liver function be monitored during meloxicam treatment?
Healthcare providers often recommend baseline liver function tests before starting meloxicam and periodic monitoring during treatment, especially for long-term users or those with risk factors. The frequency of monitoring depends on individual patient circumstances.
What precautions can help reduce the risk of liver injury from meloxicam?
Key precautions include taking the lowest effective dose for the shortest necessary duration, avoiding alcohol, maintaining regular medical check-ups, promptly reporting concerning symptoms, and ensuring your healthcare provider knows about all medications and supplements you're taking.