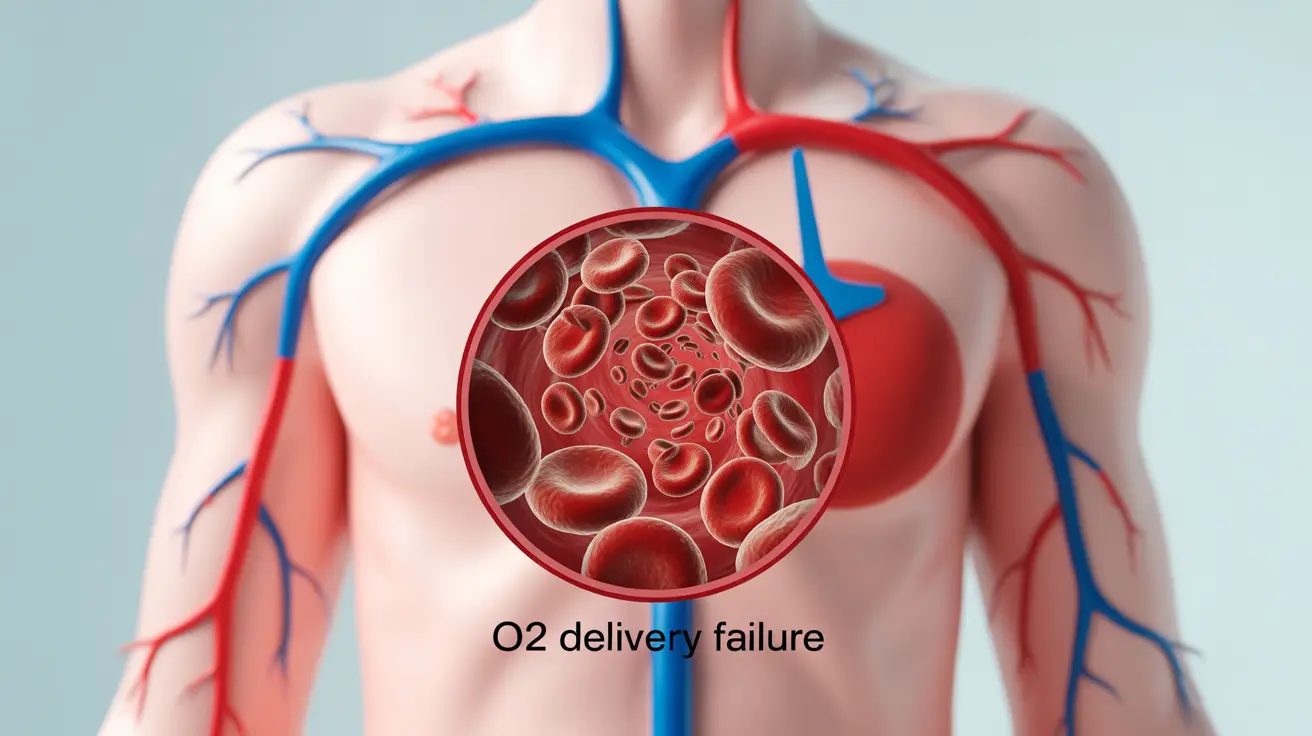
Methemoglobinemia is a serious blood disorder where abnormally high levels of methemoglobin affect the body's ability to deliver oxygen effectively to tissues. This condition can be inherited or acquired through exposure to certain chemicals or medications, making it crucial to recognize its symptoms early for proper treatment.
Whether you're concerned about potential exposure or have a family history of this condition, understanding the symptoms and treatment options is essential for managing this blood disorder effectively.
Key Symptoms of Methemoglobinemia
The symptoms of methemoglobinemia typically appear in relation to how much methemoglobin is present in the blood. Common signs include:
- Bluish or gray skin coloration (cyanosis)
- Shortness of breath
- Fatigue and weakness
- Headache
- Dizziness
- Rapid heart rate
- Confusion or altered mental status
In severe cases, when methemoglobin levels exceed 50%, patients may experience:
- Seizures
- Coma
- Life-threatening complications
Causes and Risk Factors
Methemoglobinemia can develop through various mechanisms:
Inherited Causes
Some people are born with genetic variations that affect their body's ability to maintain normal methemoglobin levels. These inherited forms can result from mutations in specific enzymes or hemoglobin proteins.
Acquired Causes
More commonly, methemoglobinemia develops after exposure to certain substances:
- Certain antibiotics
- Local anesthetics
- Nitrates in well water
- Some foods high in nitrates
- Industrial chemicals
- Dyes and inks
Diagnostic Approaches
Healthcare providers use several methods to diagnose methemoglobinemia:
- Blood gas analysis
- Co-oximetry testing
- Genetic testing (for inherited cases)
- Clinical examination of symptoms
Quick diagnosis is crucial as severe cases require immediate treatment to prevent complications.
Treatment Options
The primary treatment approaches include:
Immediate Interventions
For severe cases, methylene blue is the standard treatment, administered intravenously to quickly reduce methemoglobin levels. However, this treatment isn't suitable for everyone, particularly those with G6PD deficiency.
Supportive Care
Additional treatments may include:
- Oxygen therapy
- Removal of triggering substances
- Management of underlying conditions
- Regular monitoring of methemoglobin levels
Prevention and Management
Several strategies can help prevent or manage methemoglobinemia:
- Avoiding known trigger substances
- Regular medical check-ups if you have a family history
- Proper water testing if using well water
- Understanding medication risks
- Having an emergency plan if you're susceptible
Frequently Asked Questions
What are the symptoms of methemoglobinemia and how do they differ based on the level of methemoglobin in the blood? The symptoms progress from mild to severe as methemoglobin levels increase. At 10-20%, patients typically experience cyanosis and fatigue. At 20-50%, symptoms include headaches, dizziness, and shortness of breath. Above 50%, severe complications like seizures and coma can occur.
How is methemoglobinemia typically diagnosed, and what tests are commonly used to confirm the condition? Diagnosis primarily relies on blood gas analysis and co-oximetry testing. These tests can measure the exact percentage of methemoglobin in the blood. Physical examination showing cyanosis that doesn't improve with oxygen therapy is also a key diagnostic indicator.
What are the most effective treatments for methemoglobinemia, and when is methylene blue used? Methylene blue is the primary treatment for severe cases, administered when methemoglobin levels are significantly elevated or when patients are symptomatic. It's given intravenously and typically works within 30-60 minutes. Alternative treatments are used for patients who can't receive methylene blue.
Can certain medications or foods cause methemoglobinemia, and what are the common triggers? Yes, various substances can trigger methemoglobinemia, including certain antibiotics, local anesthetics, nitrate-rich foods, contaminated well water, and industrial chemicals. Some common medications include benzocaine, lidocaine, and dapsone.
How can I prevent or manage methemoglobinemia if I have a history of exposure to triggers or a family history of the condition? Prevention involves avoiding known triggers, regular medical monitoring, testing well water for nitrates, and maintaining awareness of medication risks. Those with a family history should inform healthcare providers and may need genetic counseling. Having an emergency plan and medical alert identification is also recommended.