Retinal microaneurysms are tiny bulges that form in the blood vessels of the retina, often serving as the earliest detectable sign of diabetic retinopathy. These small vascular changes can significantly impact eye health, particularly in people living with diabetes. Understanding their significance, detection, and management is crucial for preserving vision and maintaining overall eye health.
While these microscopic changes might seem minor, they represent an important warning sign that requires attention and proper medical care. Early detection and management of retinal microaneurysms can help prevent more serious complications and protect your vision for the future.
What Are Retinal Microaneurysms?
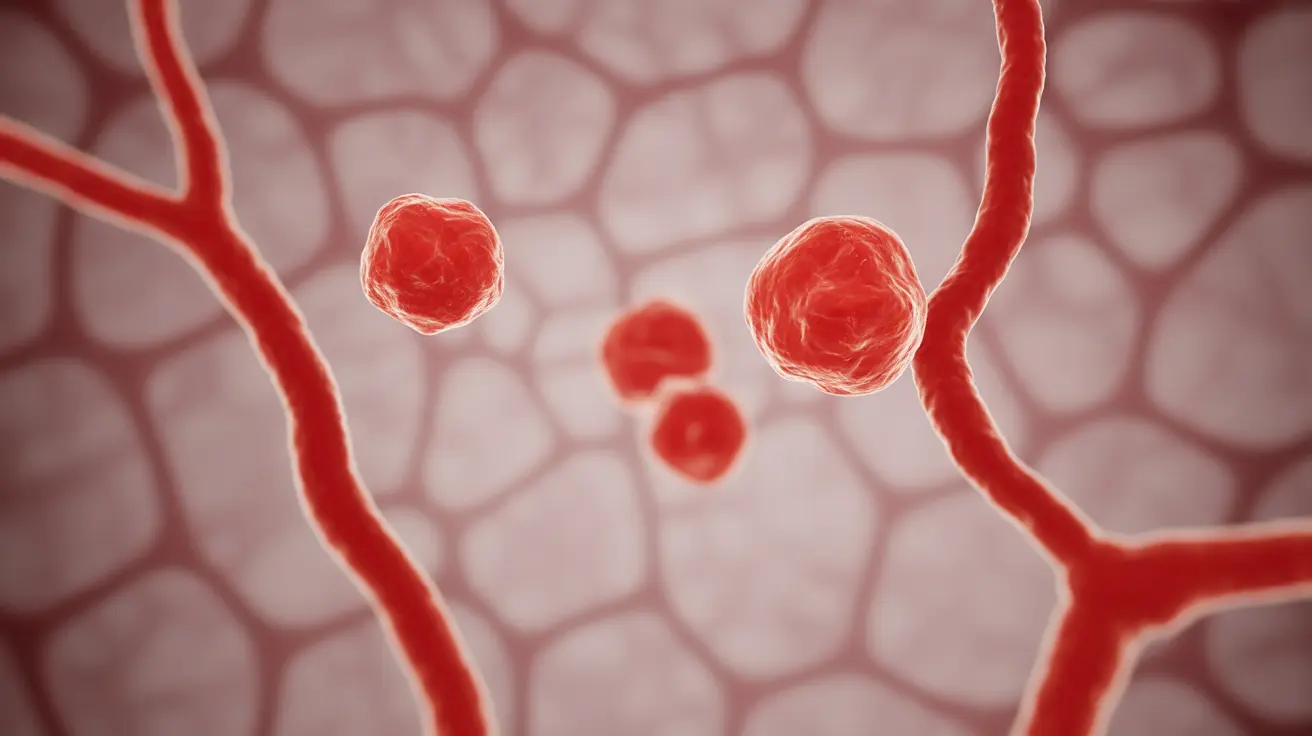
Retinal microaneurysms are microscopic outpouchings or dilations that develop in the tiny blood vessels (capillaries) of the retina. These weakened areas in blood vessel walls typically appear as small, round, red dots during eye examination. They occur when high blood sugar levels damage the walls of retinal blood vessels, causing them to balloon out in specific areas.
These vascular changes typically measure between 12 to 100 micrometers in diameter, making them virtually impossible to detect without specialized medical equipment. While small in size, their presence often indicates the beginning stages of diabetic retinopathy, a serious condition that can threaten vision if left untreated.
Early Detection and Diagnosis
Eye care professionals use several sophisticated methods to detect and monitor retinal microaneurysms:
- Dilated eye examination
- Fluorescein angiography
- Optical coherence tomography (OCT)
- Digital retinal photography
Regular screening is essential, particularly for individuals with diabetes. These examinations can detect microaneurysms before they cause noticeable symptoms, allowing for earlier intervention and better outcomes.
Impact on Vision and Health
While individual microaneurysms may not immediately affect vision, their presence can lead to several complications:
- Retinal bleeding
- Fluid accumulation in the retina
- Vision distortion
- Potential vision loss if left untreated
Understanding these potential complications emphasizes the importance of regular eye examinations and proper blood sugar management for people with diabetes.
Treatment Approaches
Treatment for retinal microaneurysms typically focuses on managing the underlying condition - usually diabetes - and may include:
- Strict blood sugar control
- Blood pressure management
- Laser photocoagulation in specific cases
- Anti-VEGF injections when necessary
- Regular monitoring and follow-up care
Prevention Strategies
Preventing or minimizing the development of retinal microaneurysms involves several key strategies:
- Maintaining optimal blood sugar levels
- Regular blood pressure monitoring
- Following a healthy diet
- Regular exercise
- Scheduling routine eye examinations
- Quitting smoking if applicable
Frequently Asked Questions
What are microaneurysms in the retina and how do they relate to diabetic retinopathy?
Microaneurysms are small bulges in retinal blood vessels that typically appear as the first visible sign of diabetic retinopathy. They occur when high blood sugar levels weaken blood vessel walls, causing them to balloon outward in small areas.
What symptoms might indicate the presence of retinal microaneurysms in diabetic patients?
Early microaneurysms often don't cause noticeable symptoms. However, as they progress, patients might experience blurred vision, floating spots, or changes in color perception. Regular eye examinations are crucial for early detection before symptoms develop.
How are microaneurysms in the retina diagnosed during an eye exam?
Eye care professionals diagnose microaneurysms through dilated eye examinations, fluorescein angiography, and specialized imaging techniques like OCT. These methods allow doctors to see the tiny blood vessel changes that aren't visible to the naked eye.
What treatments are available to manage microaneurysms and prevent vision loss?
Treatment primarily focuses on controlling diabetes through proper blood sugar management. In some cases, laser treatment or anti-VEGF injections may be necessary. Regular monitoring and early intervention are key components of successful treatment.
How can people with diabetes reduce their risk of developing microaneurysms and diabetic retinopathy?
People with diabetes can reduce their risk by maintaining tight blood sugar control, keeping blood pressure in check, following a healthy diet, exercising regularly, and attending all scheduled eye examinations. Lifestyle modifications and medication compliance are crucial preventive measures.