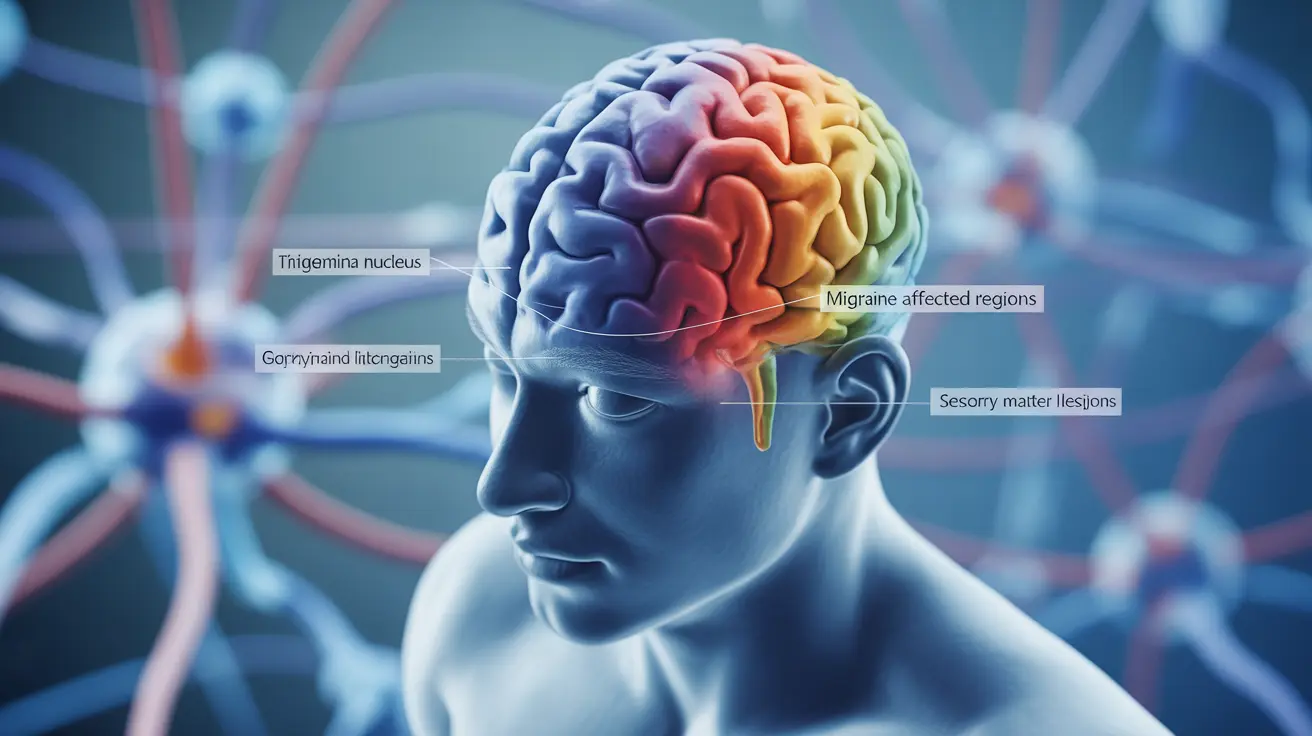
When it comes to understanding migraines, medical imaging has revealed fascinating differences between the brains of people who experience migraines and those who don't. Advanced MRI technology now allows researchers and healthcare providers to examine these distinct characteristics in unprecedented detail, offering valuable insights into how migraines affect brain structure and function.
These neurological differences not only help explain migraine symptoms but also contribute to our understanding of how this complex condition develops and progresses over time. Let's explore the key distinctions that MRI scans reveal and what they mean for migraine patients.
Structural Differences in Migraine Brains
MRI scans have identified several notable structural variations in the brains of people who experience migraines. The most significant differences include changes in gray matter volume, cortical thickness, and the presence of white matter lesions.
Gray Matter Changes
People with chronic migraines often show variations in gray matter volume in specific brain regions, particularly those involved in pain processing and sensory integration. These changes are most notable in areas responsible for:
- Pain perception and modulation
- Visual processing
- Emotional regulation
- Sensory integration
White Matter Lesions
White matter lesions appear as bright spots on MRI scans and are more common in migraine sufferers. While these lesions don't typically cause immediate cognitive problems, their presence helps doctors understand the long-term effects of recurring migraines on brain tissue.
Functional Brain Differences
Beyond structural variations, functional MRI studies have revealed differences in how migraine brains process information and respond to stimuli compared to non-migraine brains.
Neural Activity Patterns
Migraine sufferers often show distinct patterns of neural activation, particularly in response to sensory stimuli. These differences may explain why migraine patients are more sensitive to light, sound, and other environmental triggers.
Pain Processing Networks
The pain-processing networks in migraine brains show altered connectivity patterns, which may contribute to the intensity and frequency of migraine attacks. These changes can affect how pain signals are transmitted and processed throughout the brain.
Clinical Implications of Brain Differences
Understanding these brain differences has important implications for migraine diagnosis, treatment, and management. Healthcare providers can use this information to:
- Develop more targeted treatment approaches
- Monitor disease progression
- Evaluate treatment effectiveness
- Better understand individual patient needs
Frequently Asked Questions
What differences do MRI scans show between the brains of people with migraine and those without? MRI scans reveal differences in gray matter volume, white matter integrity, and neural connectivity patterns. Migraine sufferers often show changes in areas controlling pain processing, sensory integration, and emotional regulation.
Can migraines cause lasting brain damage or affect brain function as seen on MRI? While migraines can cause visible changes on MRI scans, most structural changes don't typically result in permanent damage or significant cognitive impairment. However, regular monitoring may be recommended for patients with frequent or severe migraines.
What are white matter lesions in migraine, and do they lead to cognitive problems? White matter lesions are small bright spots visible on MRI scans, more common in migraine sufferers. While their presence raises concerns, research suggests they rarely cause significant cognitive problems in most migraine patients.
How do structural and functional brain changes in migraine brains influence migraine symptoms or progression? Brain changes can affect pain processing, sensory sensitivity, and emotional regulation, potentially influencing migraine frequency and intensity. These alterations may also impact how individuals respond to different treatments.
Is MRI useful for diagnosing migraine or just for ruling out other brain conditions? MRI is primarily used to exclude other neurological conditions rather than diagnose migraines directly. However, it can help healthcare providers understand individual patient characteristics and monitor disease progression over time.