Neck pain is a common but often overlooked symptom that affects many individuals living with multiple sclerosis (MS). This challenging symptom can significantly impact daily activities and quality of life, making it crucial to understand its causes, recognize its manifestations, and explore effective management strategies.
For those with MS, neck pain can manifest in various ways and may be accompanied by other neurological symptoms. Understanding the connection between MS and neck pain is the first step toward finding relief and maintaining better overall health.
Understanding the Causes of MS-Related Neck Pain
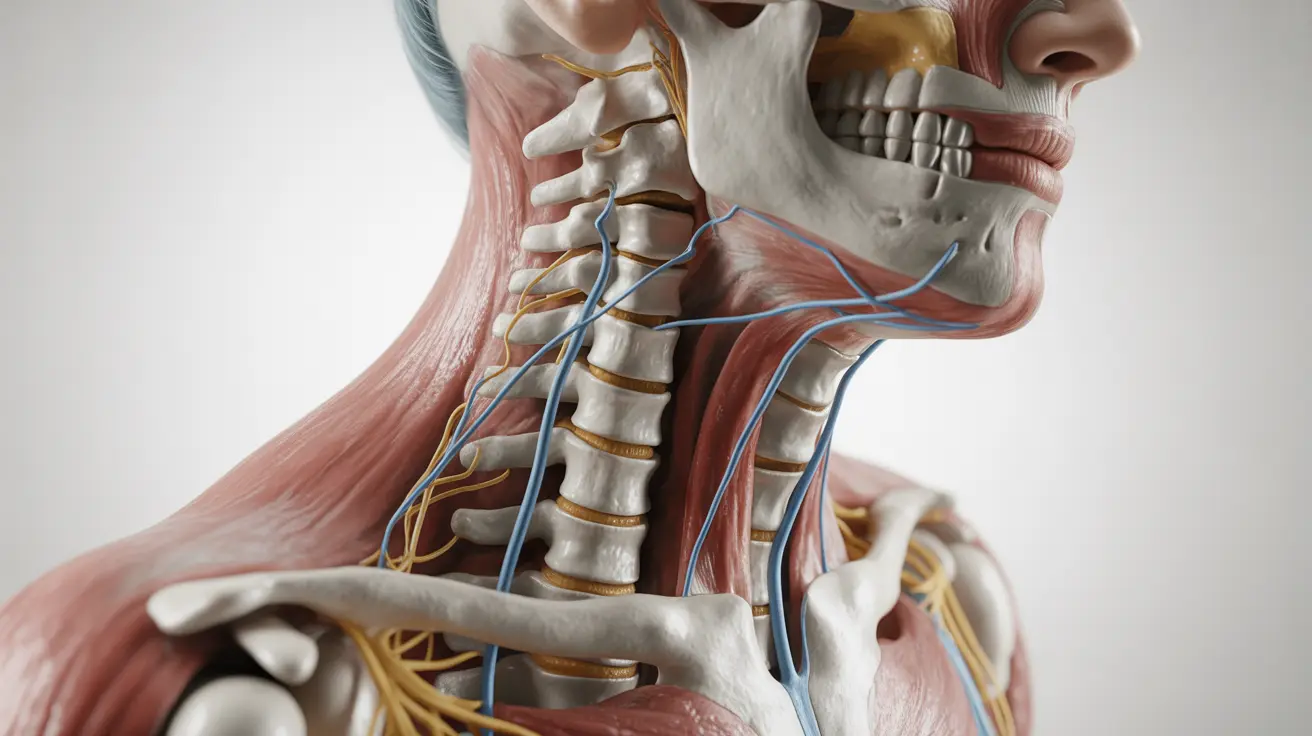
Multiple sclerosis can trigger neck pain through several mechanisms. The primary cause often stems from the disease's effect on the central nervous system, where damage to the myelin sheath disrupts normal nerve signaling. This can lead to:
- Muscle spasticity in the neck region
- Nerve pain (neuropathic pain)
- Inflammation affecting the cervical spine
- Postural changes due to muscle weakness
Additionally, chronic stress and anxiety, which are common in MS patients, can contribute to increased muscle tension in the neck area, exacerbating existing pain.
Common Symptoms and Warning Signs
Typical Manifestations
MS-related neck pain can present in various ways, including:
- Sharp, shooting pains
- Dull, persistent aches
- Stiffness and reduced range of motion
- Muscle spasms
- Radiating pain into the shoulders or arms
Lhermitte's Sign
A distinctive symptom associated with MS is Lhermitte's sign, characterized by an electric shock-like sensation that runs down the spine when bending the neck forward. This symptom often indicates active inflammation or damage in the cervical spine region.
Diagnostic Approaches and Medical Evaluation
Healthcare providers typically use a combination of methods to assess MS-related neck pain:
- Detailed medical history review
- Physical examination
- MRI scans to check for active lesions
- Neurological assessments
- Range of motion tests
Treatment Strategies and Pain Management
Medical Interventions
Several medical treatments can help manage MS-related neck pain:
- Anti-inflammatory medications
- Muscle relaxants
- Anticonvulsant medications for nerve pain
- Targeted physical therapy
- Steroid treatments for acute flares
Natural and Physical Therapy Approaches
Complementary treatments often provide significant relief:
- Gentle stretching exercises
- Posture improvement techniques
- Heat and cold therapy
- Massage therapy
- Mindfulness and relaxation techniques
Frequently Asked Questions
What causes neck pain and stiffness in people with multiple sclerosis? Neck pain in MS results from nerve damage, muscle spasticity, inflammation in the cervical spine, and postural changes due to muscle weakness. Stress and anxiety can also contribute to increased muscle tension.
What are the common symptoms of neck pain related to MS, including Lhermitte's sign? Common symptoms include sharp or dull pain, stiffness, reduced range of motion, and muscle spasms. Lhermitte's sign, a distinctive electric shock-like sensation running down the spine when bending the neck, is a characteristic symptom of MS.
How is MS-related neck pain diagnosed and treated by doctors? Doctors diagnose MS-related neck pain through medical history review, physical examination, MRI scans, and neurological assessments. Treatment typically involves a combination of medications, physical therapy, and specialized exercises.
What natural remedies and physical therapies can help relieve neck pain in MS? Natural remedies include gentle stretching, posture improvement, heat and cold therapy, massage, and mindfulness techniques. Physical therapy can help strengthen muscles and improve flexibility.
Can medications like anticonvulsants or muscle relaxants effectively manage MS neck pain? Yes, both anticonvulsants and muscle relaxants can be effective in managing MS-related neck pain. Anticonvulsants help with nerve pain, while muscle relaxants can reduce spasticity and muscle tension.