Multiple sclerosis (MS) and atherosclerosis are two distinct medical conditions that can significantly impact a person's health and quality of life. While they affect different body systems, recent research suggests potential connections between these conditions that deserve attention, particularly for individuals managing MS.
Understanding how these conditions interact and their shared risk factors is crucial for better disease management and prevention strategies. This article explores the relationship between MS and atherosclerosis, helping you understand the risks and ways to protect your health.
The Link Between Multiple Sclerosis and Cardiovascular Health
Research indicates that people with MS may face an increased risk of developing cardiovascular problems, including atherosclerosis. This connection stems from several factors, including inflammatory processes, shared risk factors, and the potential impact of MS treatments on cardiovascular health.
Understanding the Inflammatory Connection
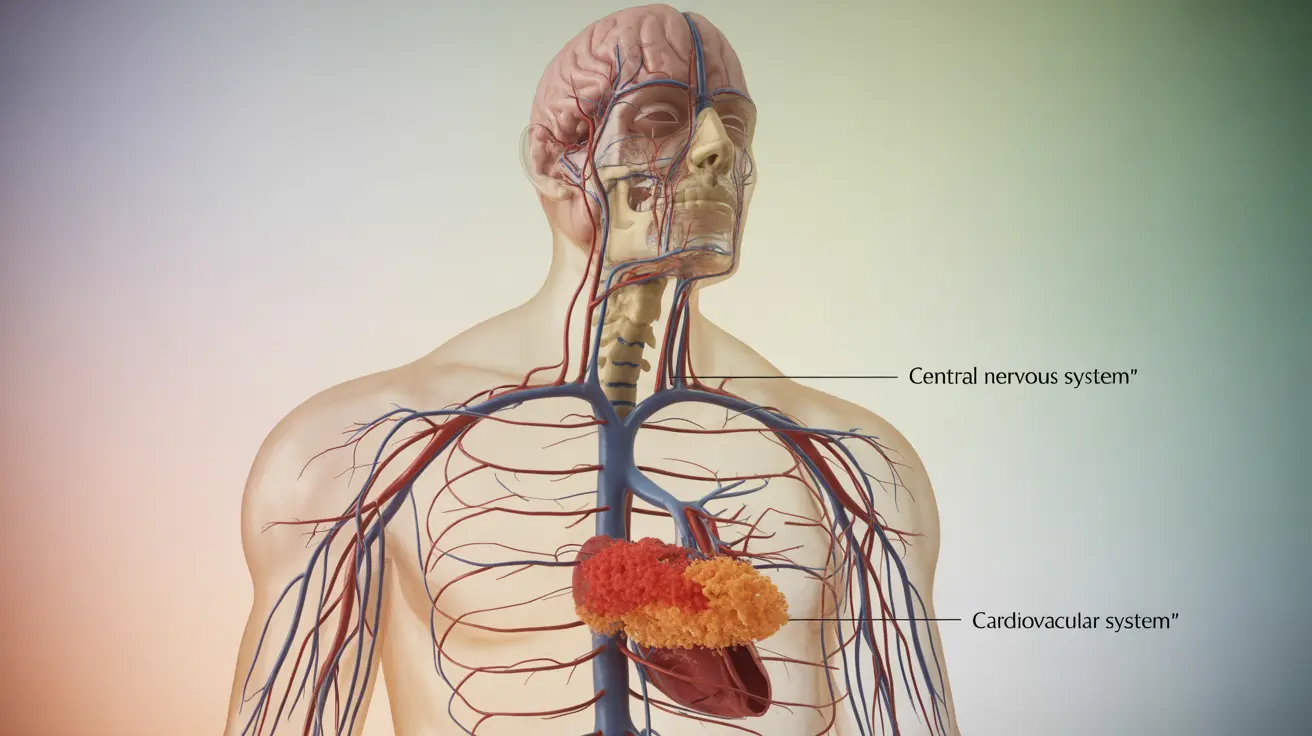
While both conditions involve inflammation, they affect the body differently. In MS, inflammation primarily targets the central nervous system, damaging the protective myelin sheath around nerve fibers. In atherosclerosis, inflammation occurs within blood vessel walls, leading to plaque buildup and narrowed arteries.
Common Risk Factors and Their Management
Several risk factors overlap between MS and atherosclerosis, including:
- Chronic inflammation
- Sedentary lifestyle
- Obesity
- Smoking
- High stress levels
- Vitamin D deficiency
Understanding these shared risk factors can help in developing comprehensive management strategies that address both conditions simultaneously.
Prevention and Management Strategies
Lifestyle Modifications
Adopting healthy lifestyle habits can help manage both conditions:
- Regular physical activity (adapted to MS limitations)
- Maintaining a healthy diet rich in anti-inflammatory foods
- Stress management techniques
- Smoking cessation
- Regular medical check-ups
Monitoring Cardiovascular Health
People with MS should pay special attention to signs of cardiovascular problems, including:
- Chest pain or pressure
- Shortness of breath
- Unusual fatigue
- Irregular heartbeat
- Dizziness or lightheadedness
Treatment Considerations
Managing both conditions requires a coordinated approach between healthcare providers. Treatment strategies should consider how medications for one condition might affect the other, and regular monitoring of both neurological and cardiovascular health is essential.
Frequently Asked Questions
Are people with multiple sclerosis at higher risk of developing atherosclerosis?
Yes, research suggests that people with MS may have an increased risk of developing atherosclerosis due to shared inflammatory processes, common risk factors, and potentially reduced physical activity levels associated with MS symptoms.
What are the shared risk factors between multiple sclerosis and atherosclerosis?
Common risk factors include chronic inflammation, sedentary lifestyle, obesity, smoking, high stress levels, and vitamin D deficiency. Managing these factors can help reduce the risk of both conditions.
How does inflammation differ in multiple sclerosis compared to atherosclerosis?
In MS, inflammation primarily affects the central nervous system, damaging myelin around nerve fibers. In atherosclerosis, inflammation occurs in blood vessel walls, leading to plaque buildup. While the inflammatory processes are different, both can contribute to overall health complications.
Can managing cardiovascular risk factors help people with multiple sclerosis reduce their risk of atherosclerosis?
Yes, managing cardiovascular risk factors through lifestyle changes, medication adherence, and regular medical monitoring can help reduce the risk of atherosclerosis in people with MS. This includes maintaining a healthy diet, staying physically active within one's abilities, and not smoking.
What symptoms should someone with multiple sclerosis watch for that might indicate atherosclerosis or heart disease?
People with MS should be alert to symptoms such as chest pain or pressure, unusual shortness of breath, excessive fatigue, irregular heartbeat, and dizziness. These symptoms should be reported to a healthcare provider promptly for evaluation.