Living with myasthenia gravis can present unique challenges, particularly when it comes to swallowing. This autoimmune condition affects the communication between nerves and muscles, potentially making eating and drinking more difficult. Understanding how to manage these symptoms is crucial for maintaining proper nutrition and quality of life.
In this comprehensive guide, we'll explore the causes of swallowing difficulties in myasthenia gravis, discuss practical strategies for safe eating and drinking, and outline when to seek medical attention.
Understanding Swallowing Problems in Myasthenia Gravis
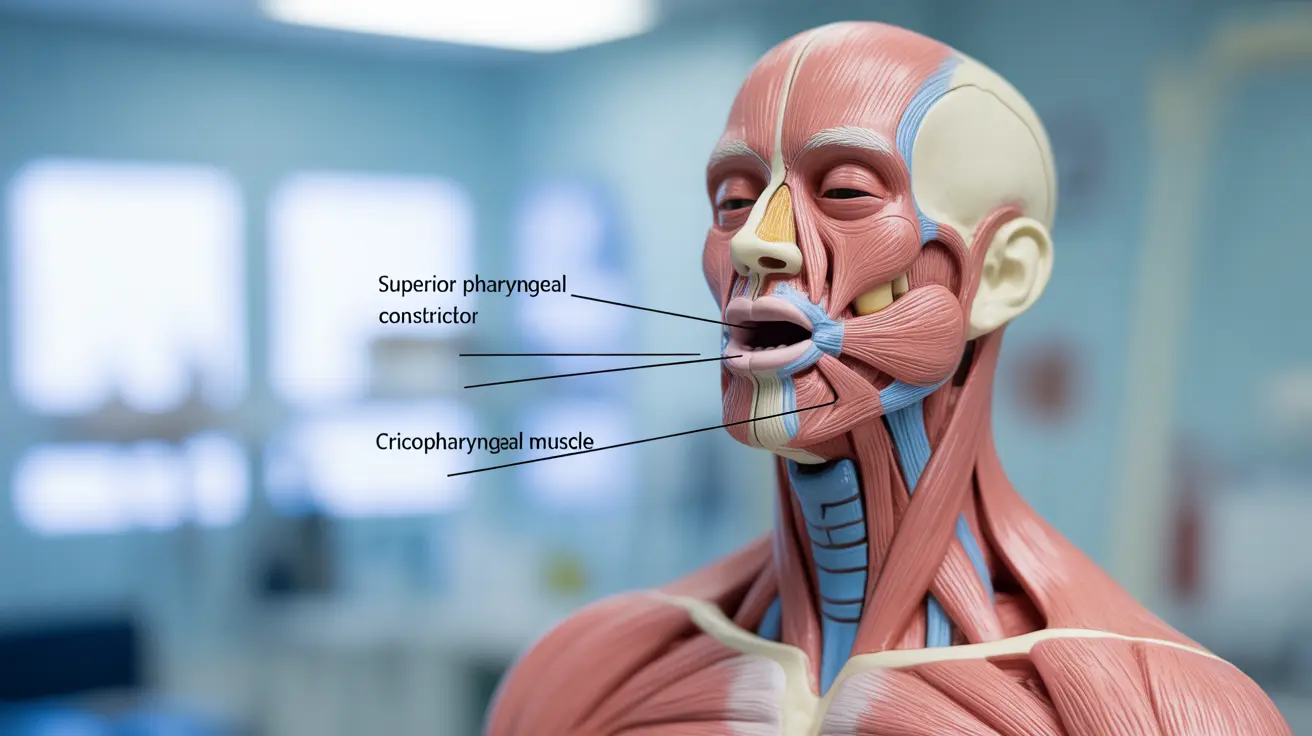
Myasthenia gravis can affect the muscles involved in swallowing, known as the bulbar muscles. When these muscles become weak, they may not coordinate properly during eating and drinking, leading to difficulties in moving food from the mouth to the stomach. This condition, known as dysphagia, can vary in severity throughout the day and may worsen with fatigue.
Safe Eating and Drinking Strategies
Timing Your Meals
Planning your meals around your medication schedule and energy levels can significantly improve your eating experience. Many people find they have better muscle strength earlier in the day or shortly after taking their medication.
Food Texture Modifications
Adjusting food textures can make swallowing safer and easier. Consider these modifications:
- Choosing soft, moist foods
- Using gravies and sauces to make foods smoother
- Avoiding dry or crumbly textures
- Cutting food into small, manageable pieces
Positioning and Posture
Proper positioning while eating can help prevent choking and make swallowing easier:
- Sit fully upright at a 90-degree angle
- Keep your head slightly tucked forward
- Take small bites and sips
- Avoid talking while eating
Foods to Avoid with Myasthenia Gravis
Certain foods may be more challenging to eat safely when experiencing swallowing difficulties:
- Hard, crunchy foods like raw vegetables or nuts
- Sticky foods like peanut butter
- Foods with mixed textures
- Very dry foods like crackers or toast
- Foods with small particles like rice or seeds
Medical Management and Treatment Options
Several medical interventions can help improve swallowing function in people with myasthenia gravis:
- Acetylcholinesterase inhibitors
- Immunosuppressive medications
- Speech and swallowing therapy
- Regular monitoring by a neurologist
- Specialized swallowing evaluations
Warning Signs and When to Seek Help
It's essential to recognize when swallowing difficulties require immediate medical attention. Watch for:
- Frequent coughing or choking while eating
- Unexplained weight loss
- Recurring chest infections
- Voice changes during meals
- Food or liquid coming through the nose
Frequently Asked Questions
What causes swallowing difficulties in people with myasthenia gravis? Swallowing difficulties occur when myasthenia gravis affects the muscles responsible for swallowing (bulbar muscles). The condition disrupts nerve signals to these muscles, making them weak and less coordinated during eating and drinking.
How can I eat and drink safely if I have myasthenia gravis-related swallowing problems? Practice safe eating by sitting upright, taking small bites, eating slowly, and modifying food textures. Time meals when medication is most effective, and focus on soft, moist foods. Avoid distractions while eating and ensure proper positioning.
What foods should I avoid if I have trouble swallowing due to myasthenia gravis? Avoid hard, crunchy foods, sticky substances, mixed textures, very dry foods, and items with small particles. These foods can be more challenging to swallow safely and may increase the risk of choking.
What medical treatments are available to improve swallowing in myasthenia gravis? Treatment options include acetylcholinesterase inhibitors, immunosuppressive medications, specialized swallowing therapy, and regular monitoring by healthcare professionals. A combination approach often yields the best results.
When should I see a doctor if swallowing issues from myasthenia gravis get worse? Seek immediate medical attention if you experience frequent choking, unexplained weight loss, recurring chest infections, voice changes during meals, or if food or liquid comes through your nose. These symptoms may indicate a need for treatment adjustment.