Neuroleptic malignant syndrome (NMS) is a rare but potentially life-threatening reaction to certain medications, particularly antipsychotic drugs. This serious condition requires immediate medical attention and can develop rapidly, sometimes within hours or days of starting or changing medication doses. Understanding its symptoms, risk factors, and treatment options is crucial for both healthcare providers and patients taking antipsychotic medications.
Key Symptoms and Development
The onset of neuroleptic malignant syndrome typically occurs within the first two weeks of starting or adjusting antipsychotic medication. The condition presents with several distinctive symptoms:
- Extremely high fever (often above 100.4°F/38°C)
- Severe muscle rigidity
- Mental status changes
- Excessive sweating
- Irregular heart rate and blood pressure
- Tremors or muscle spasms
These symptoms usually develop rapidly and can worsen quickly without proper medical intervention. Early recognition is crucial for successful treatment and recovery.
Risk Factors and Triggering Medications
Several factors can increase the risk of developing neuroleptic malignant syndrome:
High-Risk Medications
- First-generation (typical) antipsychotics
- Second-generation (atypical) antipsychotics
- Certain anti-nausea medications
- Some Parkinson's disease medications
Contributing Risk Factors
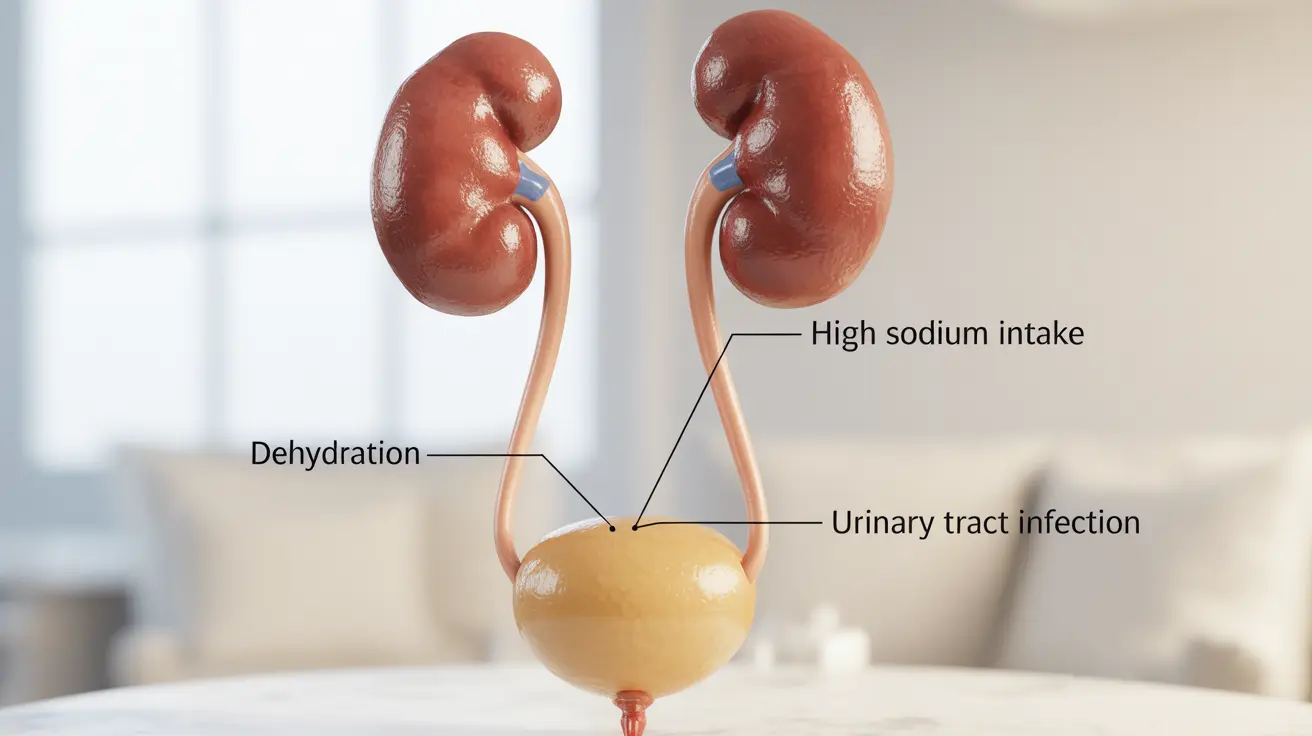
- Dehydration
- Physical exhaustion
- Previous history of NMS
- Rapid dose increases
- Male gender
- Young age
Diagnosis and Differential Considerations
Diagnosing neuroleptic malignant syndrome requires careful clinical evaluation and laboratory testing. Healthcare providers typically look for:
- Elevated creatine phosphokinase (CPK) levels
- Changes in white blood cell count
- Liver function abnormalities
- Signs of kidney dysfunction
Distinguishing NMS from similar conditions like serotonin syndrome or malignant hyperthermia is crucial for proper treatment. Each condition requires different therapeutic approaches.
Treatment Approaches
The management of neuroleptic malignant syndrome involves several key steps:
Immediate Interventions
- Discontinuation of triggering medications
- Intensive supportive care
- Temperature management
- Fluid and electrolyte replacement
Medication-Based Treatment
- Dantrolene for muscle rigidity
- Bromocriptine for symptom management
- Benzodiazepines for anxiety and agitation
Recovery and Future Considerations
Most patients can achieve full recovery from neuroleptic malignant syndrome with proper treatment. However, careful consideration is needed before resuming any antipsychotic medications. Recovery typically takes 7-14 days, though some cases may require longer hospital stays.
Frequently Asked Questions
What are the common symptoms of neuroleptic malignant syndrome and how quickly do they develop? The primary symptoms include high fever, severe muscle rigidity, mental status changes, and autonomic dysfunction. These symptoms typically develop within hours to days of starting or adjusting antipsychotic medications.
Which medications or factors increase the risk of developing neuroleptic malignant syndrome? Antipsychotic medications, particularly first-generation agents, pose the highest risk. Other risk factors include dehydration, physical exhaustion, rapid dose increases, and a previous history of NMS.
How is neuroleptic malignant syndrome diagnosed and distinguished from similar conditions like serotonin syndrome? Diagnosis involves clinical evaluation of symptoms, laboratory tests including CPK levels, and careful examination of medication history. NMS is distinguished from serotonin syndrome by its characteristic muscle rigidity and slower onset.
What are the standard treatments and supportive care measures for managing neuroleptic malignant syndrome? Treatment includes immediate discontinuation of triggering medications, intensive supportive care, temperature management, and medications like dantrolene and bromocriptine. Supportive measures include IV fluids and electrolyte management.
Can patients fully recover from neuroleptic malignant syndrome and is it safe to resume antipsychotic medications afterward? Most patients can achieve full recovery with proper treatment. Resuming antipsychotic medications requires careful consideration, usually with different medications at lower doses, and only after complete recovery.