Non seminoma testicular cancer is a serious but treatable form of testicular cancer that primarily affects young men between the ages of 15 and 35. This type of cancer develops in the germ cells of the testicles and can grow and spread more rapidly than its seminoma counterpart. Understanding its symptoms, diagnosis methods, and treatment options is crucial for early detection and successful outcomes.
Understanding Non Seminoma Testicular Cancer
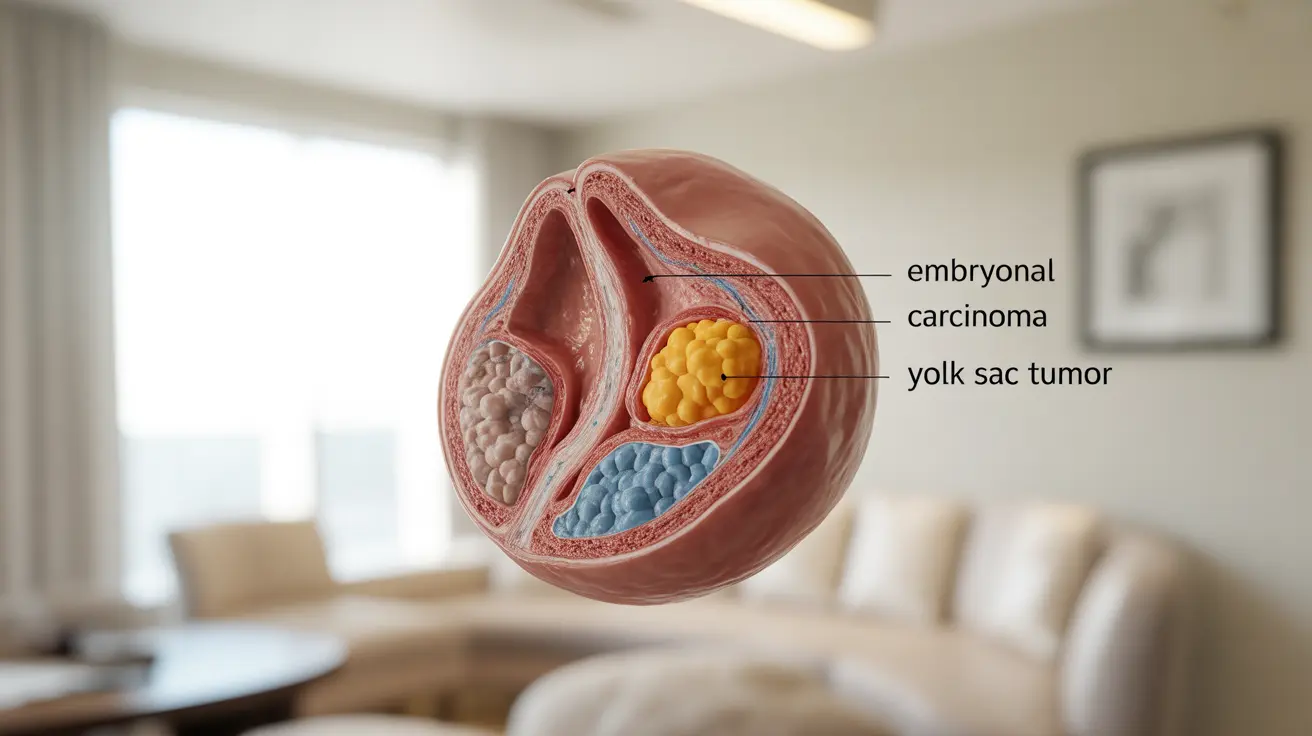
Non seminoma testicular cancer comprises several different types of cancer cells, including embryonal carcinoma, yolk sac tumors, choriocarcinoma, and teratoma. These tumors often occur in combination, making them more complex to treat than pure seminomas. The diverse nature of these tumors can affect both the treatment approach and overall prognosis.
Key Signs and Symptoms
Recognizing the early warning signs of non seminoma testicular cancer is vital for prompt diagnosis and treatment. Common symptoms include:
- A painless lump or swelling in either testicle
- A feeling of heaviness in the scrotum
- A dull ache in the lower abdomen or groin
- Sudden fluid collection in the scrotum
- Pain or discomfort in a testicle or the scrotum
- Enlargement or tenderness of the breasts
Diagnostic Process and Testing
When non seminoma testicular cancer is suspected, healthcare providers typically follow a comprehensive diagnostic approach that includes:
- Physical examination
- Ultrasound imaging of the testicles
- Blood tests for tumor markers (AFP, beta-hCG, and LDH)
- CT scans of the chest, abdomen, and pelvis
- Testicular biopsy (if necessary)
Treatment Approaches
Treatment for non seminoma testicular cancer varies depending on the stage and extent of the disease. Common treatment options include:
Surgery
Radical inguinal orchiectomy is typically the first step in treatment, involving the removal of the affected testicle through an incision in the groin.
Chemotherapy
Multiple cycles of chemotherapy may be necessary, especially if the cancer has spread beyond the testicle. The BEP regimen (bleomycin, etoposide, and cisplatin) is commonly used.
Radiation Therapy
While less common in non seminoma cases, radiation therapy might be used in specific situations, particularly if there are remaining cancer cells after surgery.
Prognosis and Survival Rates
The prognosis for non seminoma testicular cancer is generally favorable, especially when caught early. Five-year survival rates vary by stage:
- Stage I: Nearly 100%
- Stage II: 90-95%
- Stage III: 70-80%
Frequently Asked Questions
What are the common symptoms and signs of non seminoma testicular cancer?
Common symptoms include a painless lump or swelling in the testicle, heaviness in the scrotum, dull abdominal or groin pain, and occasional breast tenderness or enlargement. Any unusual changes should be evaluated by a healthcare provider promptly.
How is non seminoma testicular cancer diagnosed and what tests are involved?
Diagnosis typically involves physical examination, ultrasound imaging, blood tests for tumor markers (AFP, beta-hCG, LDH), and CT scans. In some cases, a testicular biopsy may be necessary for confirmation.
What treatment options are available for non seminoma testicular cancer?
Treatment options include surgery (radical inguinal orchiectomy), chemotherapy (typically BEP protocol), and sometimes radiation therapy. The specific treatment plan depends on the cancer stage and individual factors.
How does prognosis and survival rate vary by stage in non seminoma testicular cancer?
Survival rates are excellent for early-stage disease (nearly 100% for Stage I), very good for Stage II (90-95%), and good for Stage III (70-80%). Early detection and treatment significantly improve outcomes.
What is the difference between non seminoma and seminoma testicular cancer?
Non seminomas typically grow and spread more quickly than seminomas and often contain multiple types of cancer cells. They generally affect younger men and may require more aggressive treatment approaches compared to seminomas, which are typically more sensitive to radiation therapy.