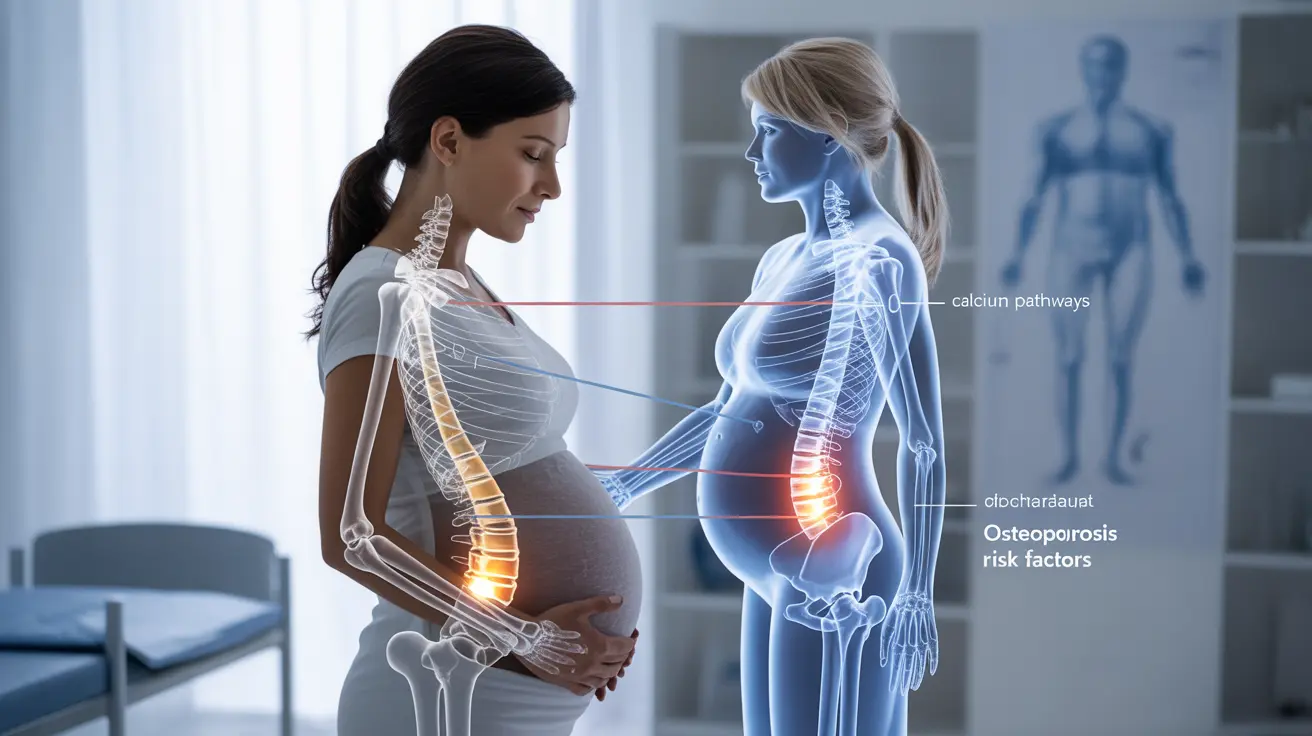
Pregnancy brings numerous changes to a woman's body, and bone health can be significantly affected during this time. When osteoporosis occurs during or shortly after pregnancy, it presents unique challenges that require careful medical attention and management. Understanding the relationship between osteoporosis and pregnancy is crucial for expectant mothers and healthcare providers alike.
While pregnancy-associated osteoporosis is relatively rare, its impact can be significant, potentially affecting both maternal health and pregnancy outcomes. This comprehensive guide explores the essential aspects of managing osteoporosis during pregnancy, including symptoms, risk factors, and treatment options.
Understanding Pregnancy-Associated Osteoporosis
Pregnancy-associated osteoporosis is a rare condition that typically develops during late pregnancy or in the early postpartum period. During pregnancy, a woman's body undergoes significant calcium demands to support fetal bone development, which can sometimes lead to temporary changes in bone density.
The condition most commonly affects the spine and hip bones, although it can impact other areas of the skeleton as well. Understanding these changes is crucial for proper diagnosis and management.
Signs and Symptoms to Watch For
The symptoms of pregnancy-associated osteoporosis can vary in severity and may include:
- Severe back pain
- Height loss
- Fractures, particularly in the vertebrae
- Difficulty walking or moving
- Postural changes
- Pain that worsens with weight-bearing activities
Risk Factors and Causes
Several factors can increase the risk of developing osteoporosis during pregnancy:
- Family history of osteoporosis
- Previous fractures
- Low body weight
- Smoking
- Limited physical activity
- Vitamin D deficiency
- Certain medical conditions affecting bone metabolism
Diagnosis and Testing
Diagnosing osteoporosis during pregnancy presents unique challenges due to concerns about radiation exposure. Healthcare providers typically rely on:
- Medical history evaluation
- Physical examination
- MRI imaging (when necessary)
- Blood tests to check calcium and vitamin D levels
- Bone density testing after pregnancy
Treatment Approaches During Pregnancy
Managing osteoporosis during pregnancy requires a careful balance between protecting maternal bone health and ensuring fetal safety. Treatment options may include:
- Calcium and vitamin D supplementation
- Physical therapy
- Safe exercise programs
- Pain management techniques
- Careful monitoring throughout pregnancy
Prevention and Lifestyle Modifications
Several preventive measures can help maintain bone health during pregnancy:
- Regular, safe exercise as approved by healthcare providers
- Adequate calcium-rich diet
- Proper vitamin D intake
- Avoiding smoking and alcohol
- Maintaining good posture
- Using proper body mechanics
Postpartum Care and Recovery
After delivery, continued monitoring and management are essential. This may include:
- Bone density testing
- Continued supplementation
- Gradual return to weight-bearing exercises
- Regular medical follow-up
- Careful consideration of breastfeeding options
Frequently Asked Questions
What are the common symptoms of osteoporosis during pregnancy and how is it diagnosed?
Common symptoms include severe back pain, height loss, and difficulty with movement. Diagnosis typically involves careful medical history evaluation, physical examination, and selective use of MRI imaging, as traditional bone density scans are usually avoided during pregnancy.
What causes pregnancy-associated osteoporosis and who is at risk of developing it?
The exact cause isn't fully understood, but risk factors include family history, previous fractures, low body weight, and vitamin D deficiency. Women with pre-existing bone conditions or certain metabolic disorders are at higher risk.
How is osteoporosis during pregnancy treated and what are the safe medication options?
Treatment typically focuses on calcium and vitamin D supplementation, physical therapy, and safe exercise programs. Most osteoporosis medications are avoided during pregnancy, with treatment decisions made on a case-by-case basis.
Can women with osteoporosis have a healthy pregnancy and what precautions should they take?
Yes, women with osteoporosis can have healthy pregnancies with proper medical supervision. Precautions include regular medical monitoring, appropriate supplementation, and following safe exercise guidelines.
Does breastfeeding affect bone loss or recovery related to pregnancy-associated osteoporosis?
Breastfeeding can temporarily increase bone loss, but most women recover their bone density after weaning. Healthcare providers may recommend additional calcium supplementation and monitoring during this period.