Many people wonder about the relationship between osteoporosis and autoimmune conditions, especially since both can significantly impact overall health. While osteoporosis itself is primarily a bone disorder rather than an autoimmune disease, there are important connections between these conditions that deserve attention.
Understanding how autoimmune diseases and osteoporosis interact is crucial for proper diagnosis, treatment, and prevention strategies. This comprehensive guide explores the relationship between these conditions and provides essential information for those affected by either or both conditions.
The Nature of Osteoporosis
Osteoporosis is fundamentally a skeletal disorder characterized by decreased bone density and compromised bone strength. Unlike autoimmune diseases, which involve the immune system attacking healthy tissues, osteoporosis primarily results from an imbalance in bone remodeling processes.
The condition occurs when bone breakdown (resorption) happens faster than bone formation, leading to increased fracture risk and reduced bone strength. While not autoimmune in nature, various autoimmune conditions can significantly influence its development.
The Immune System's Role in Bone Health
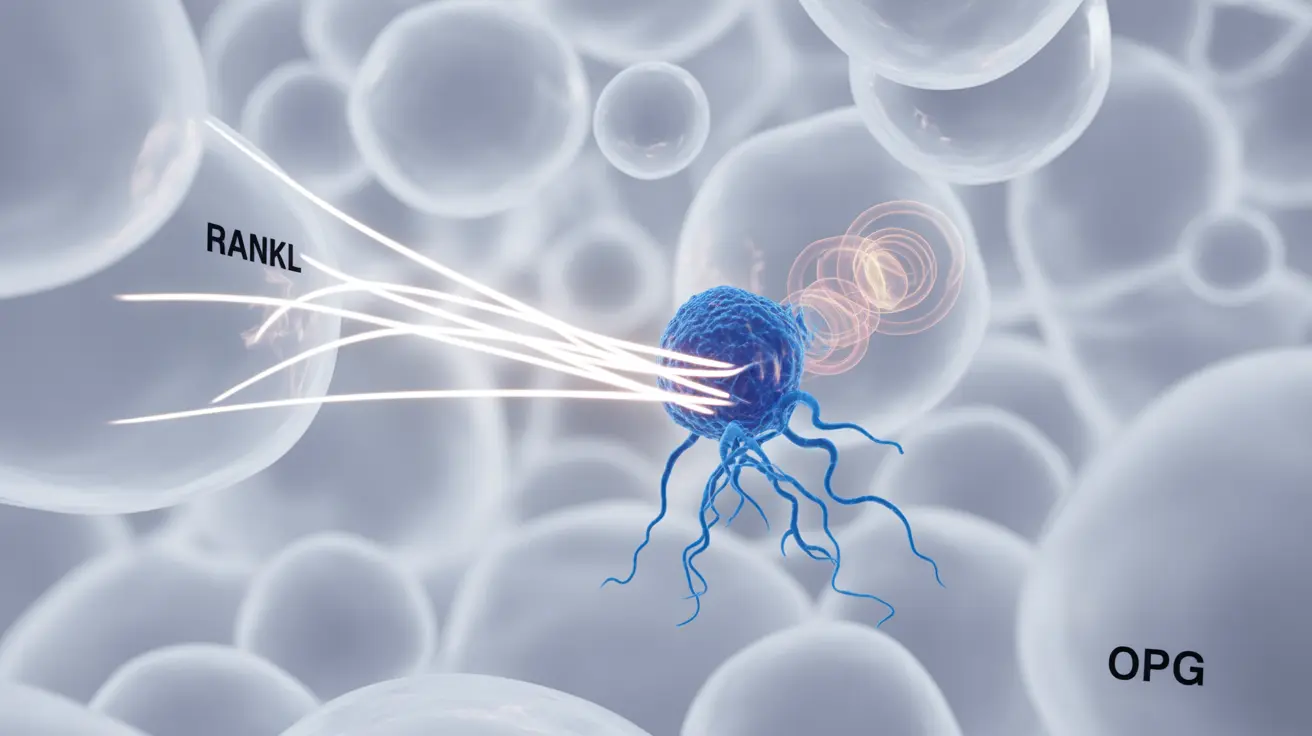
Recent research has revealed fascinating connections between the immune system and bone health. The field of osteoimmunology studies how immune cells and bone cells communicate and influence each other.
- Inflammatory cytokines that can accelerate bone loss
- Immune cells that influence bone-forming osteoblasts and bone-resorbing osteoclasts
- Shared signaling pathways between immune and bone cells
Autoimmune Diseases and Osteoporosis Risk
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Multiple sclerosis
- Inflammatory bowel disease
These conditions can affect bone health through various mechanisms, including chronic inflammation, reduced physical activity, and the effects of medications used to treat these conditions.
Medication Impact on Bone Health
Many medications used to treat autoimmune diseases can affect bone density. Corticosteroids, commonly prescribed for various autoimmune conditions, are particularly notable for their potential to cause rapid bone loss when used long-term.
Other medications may have protective effects on bone health, making it essential to work closely with healthcare providers to balance treatment benefits and risks.
Prevention and Management Strategies
- Regular bone density monitoring
- Adequate calcium and vitamin D intake
- Weight-bearing exercise when appropriate
- Lifestyle modifications like smoking cessation
- Regular medical check-ups
Frequently Asked Questions
Is osteoporosis considered an autoimmune disease or a bone condition?
Osteoporosis is primarily a bone condition, not an autoimmune disease. It's characterized by decreased bone density and structural deterioration of bone tissue, rather than an immune system attack on healthy tissues.
How do autoimmune diseases like rheumatoid arthritis increase the risk of osteoporosis?
Autoimmune diseases increase osteoporosis risk through chronic inflammation, reduced physical activity, and the side effects of medications like corticosteroids. The inflammatory processes can directly impact bone metabolism and accelerate bone loss.
What role does the immune system play in bone health and osteoporosis development?
The immune system influences bone health through various mechanisms, including the production of inflammatory molecules that affect bone formation and resorption. This interaction is studied in the field of osteoimmunology.
Can medications for autoimmune diseases affect bone density and lead to osteoporosis?
Yes, certain medications, particularly corticosteroids, can significantly impact bone density. Long-term use of these medications may accelerate bone loss and increase the risk of developing osteoporosis.
How can people with autoimmune disorders prevent or manage osteoporosis risk?
Prevention and management strategies include regular bone density screenings, maintaining adequate calcium and vitamin D levels, engaging in appropriate exercise, and working closely with healthcare providers to optimize medication regimens while protecting bone health.