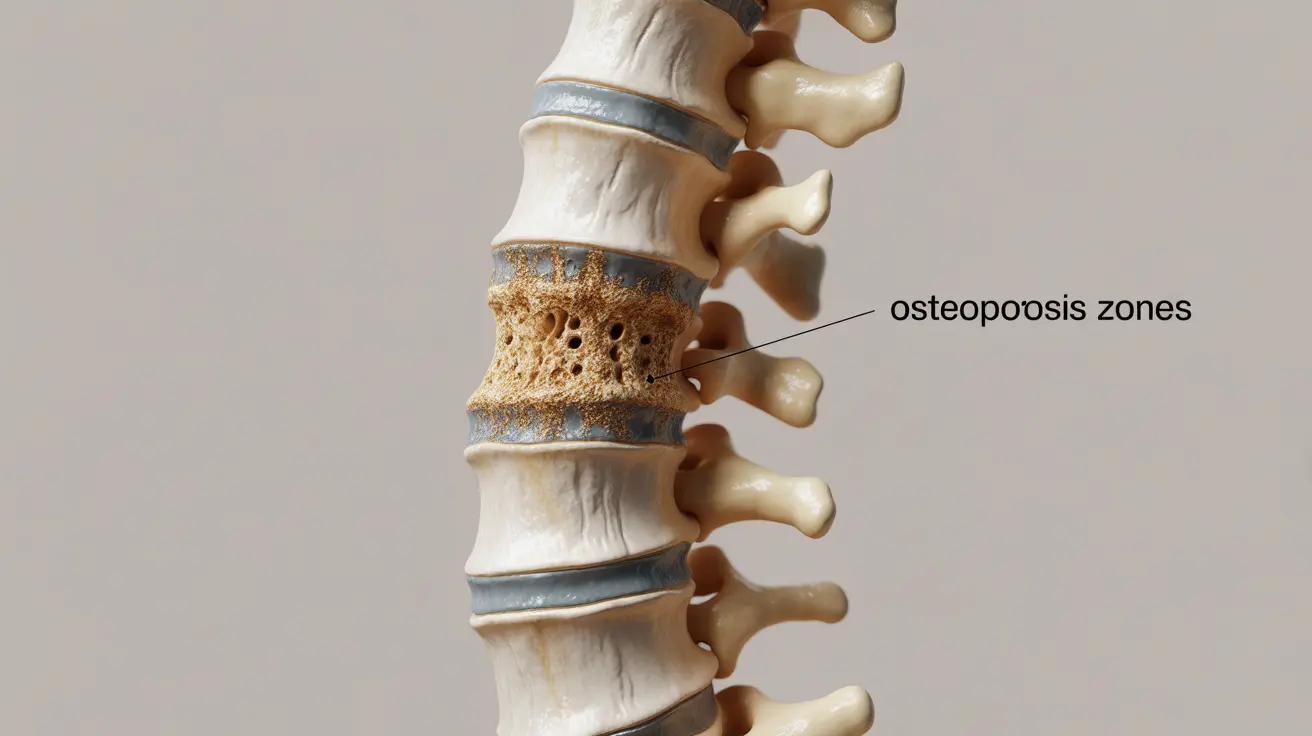
Osteoporosis of the spine represents a significant health concern that affects millions of people, particularly older adults and postmenopausal women. This condition weakens the vertebrae, making them more susceptible to fractures and potentially leading to chronic pain and reduced mobility. Understanding the available treatment options and management strategies is crucial for maintaining bone health and preventing complications.
Effective treatment typically involves a multi-faceted approach combining medication, lifestyle modifications, and preventive measures. Let's explore the various treatment options and strategies available for managing spinal osteoporosis effectively.
Medical Treatments for Spinal Osteoporosis
Several medication options have proven effective in treating osteoporosis of the spine. The most commonly prescribed medications include:
- Bisphosphonates (such as alendronate and risedronate)
- Denosumab
- Teriparatide
- Abaloparatide
- Selective Estrogen Receptor Modulators (SERMs)
These medications work by either slowing bone loss or stimulating new bone formation, helping to maintain and improve bone density in the spine.
Exercise and Physical Activity Guidelines
Regular physical activity plays a crucial role in managing spinal osteoporosis. The most beneficial exercises include:
- Weight-bearing exercises
- Resistance training
- Balance exercises
- Posture-improving activities
It's essential to work with a physical therapist or qualified fitness professional to develop a safe and effective exercise program tailored to your condition.
Nutritional Support and Supplementation
Proper nutrition is fundamental in treating osteoporosis of the spine. Key nutritional components include:
Calcium Requirements
Adults with spinal osteoporosis typically need 1,000-1,200 mg of calcium daily, obtained through diet and supplements. Good dietary sources include:
- Dairy products
- Leafy green vegetables
- Fortified foods
- Fish with bones
Vitamin D Supplementation
Vitamin D is crucial for calcium absorption and bone health. Most adults need 800-1,000 IU daily, with some requiring higher doses based on their blood levels and medical condition.
Preventing Falls and Fractures
Implementation of proper safety measures is crucial for preventing fractures. Key strategies include:
- Home modification to remove trip hazards
- Installing proper lighting
- Using assistive devices when necessary
- Wearing appropriate footwear
- Regular vision and hearing check-ups
Lifestyle Modifications
Several lifestyle changes can significantly impact the management of spinal osteoporosis:
- Quitting smoking
- Limiting alcohol consumption
- Maintaining a healthy weight
- Using proper body mechanics
- Avoiding activities that put excessive strain on the spine
Frequently Asked Questions
What are the most effective medications for treating osteoporosis of the spine?
Bisphosphonates are typically considered first-line treatment, followed by denosumab and anabolic agents like teriparatide. The choice depends on factors such as severity of the condition, other medical conditions, and individual risk factors.
How can lifestyle changes and exercise help manage spinal osteoporosis?
Regular weight-bearing exercise, proper nutrition, and maintaining good posture can help strengthen bones and muscles, improve balance, and reduce the risk of falls. These lifestyle modifications complement medical treatments and are essential for long-term management.
What are the common side effects of bisphosphonates used for spine osteoporosis?
Common side effects include gastrointestinal issues, such as heartburn and stomach pain. Rare but serious side effects can include osteonecrosis of the jaw and atypical femoral fractures. It's important to discuss potential risks with your healthcare provider.
How does calcium and vitamin D supplementation support treatment for spinal osteoporosis?
These nutrients work together to maintain bone health: calcium provides the building blocks for bone tissue, while vitamin D helps the body absorb and utilize calcium effectively. Adequate levels of both are essential for optimal treatment outcomes.
What strategies can help prevent fractures and falls in people with spinal osteoporosis?
Key strategies include home safety modifications, regular exercise to improve balance and strength, proper lighting, using assistive devices when needed, and regular vision checks. These measures, combined with medication compliance, help reduce fracture risk.