Menopause brings numerous changes to a woman's body, and one challenging symptom many women experience is overactive bladder. This condition can significantly impact quality of life, causing frequent urination, sudden urges, and potential embarrassment. Understanding the connection between menopause and bladder changes is crucial for finding effective management strategies.
In this comprehensive guide, we'll explore how hormonal changes during menopause affect bladder function and discuss various treatment options available to help women regain control and confidence.
The Menopause-Bladder Connection
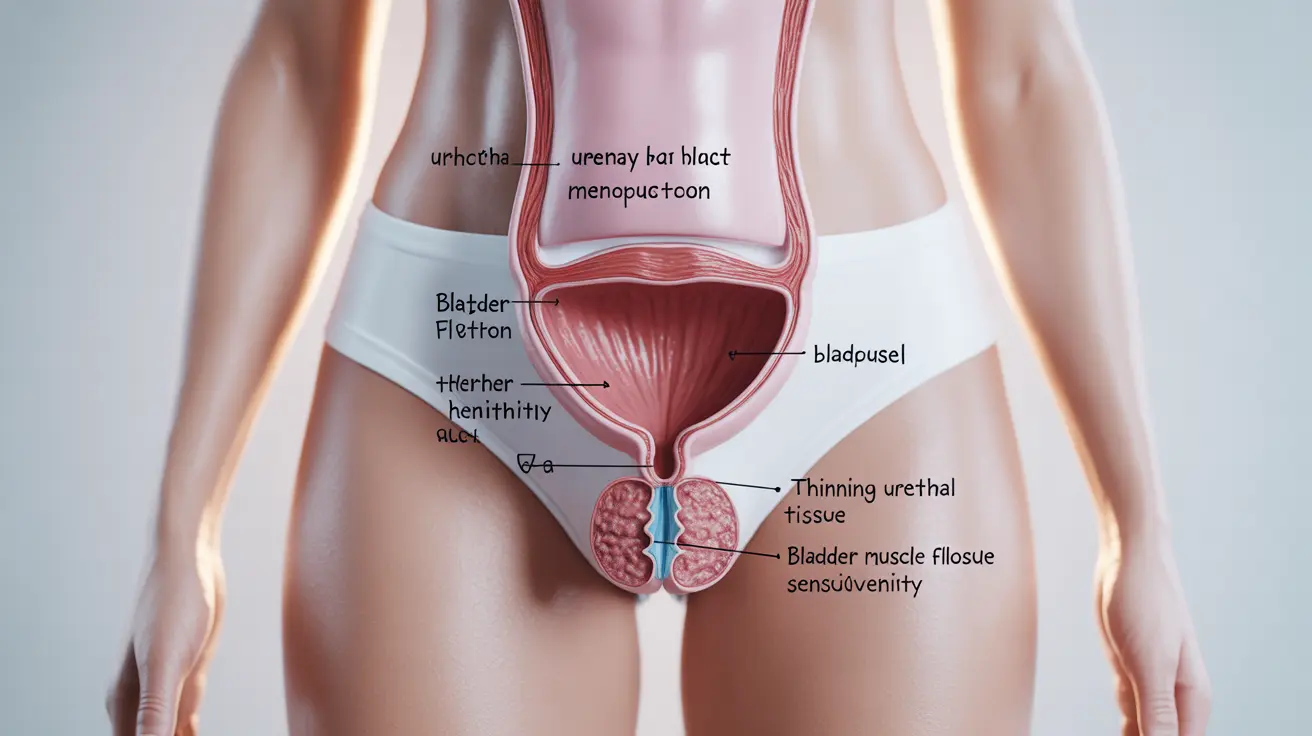
During menopause, declining estrogen levels affect the urinary tract and pelvic floor muscles in several ways. The urethral tissue becomes thinner and less elastic, while pelvic floor muscles may weaken. These changes can lead to increased urinary frequency, urgency, and sometimes incontinence.
The bladder muscle (detrusor) may become more sensitive and contract more frequently, even when the bladder isn't full. This overactivity results in sudden, strong urges to urinate that can be difficult to control.
Common Symptoms and Signs
Women experiencing overactive bladder during menopause typically report:
- Frequent urination (8 or more times daily)
- Sudden, urgent needs to urinate
- Nocturia (frequent nighttime urination)
- Difficulty holding urine after feeling the urge
- Occasional leakage or incontinence
Treatment Approaches for Menopausal Bladder Issues
Behavioral Modifications
The first line of treatment often involves lifestyle changes and behavioral techniques:
- Scheduled bathroom visits
- Double voiding techniques
- Limiting caffeine and alcohol intake
- Managing fluid intake timing
- Maintaining a healthy weight
Pelvic Floor Exercises
Kegel exercises and other pelvic floor strengthening techniques can significantly improve bladder control. These exercises help support the bladder and other pelvic organs, reducing symptoms of overactive bladder.
Medication Options
Several medications can help manage overactive bladder symptoms during menopause:
- Anticholinergics
- Beta-3 agonists
- Local estrogen therapy
- Combination treatments
Vaginal Estrogen Therapy
Local estrogen treatment can help restore urinary tract tissue health and improve bladder function. This targeted approach minimizes systemic absorption while providing effective symptom relief.
Lifestyle Management Strategies
Implementing certain lifestyle changes can significantly impact bladder control:
- Maintaining a bladder diary
- Following a balanced diet
- Staying physically active
- Managing chronic conditions
- Practicing stress reduction techniques
Frequently Asked Questions
How does menopause cause overactive bladder symptoms like urgency and frequent urination?
Menopause causes declining estrogen levels, which leads to thinning of urethral tissue and weakening of pelvic floor muscles. These changes, combined with decreased bladder elasticity, result in increased urinary frequency and urgency.
What treatments are effective for managing overactive bladder during menopause?
Effective treatments include behavioral modifications, pelvic floor exercises, medications like anticholinergics and beta-3 agonists, and local estrogen therapy. A combination approach often yields the best results.
Can pelvic floor exercises help reduce overactive bladder symptoms in menopausal women?
Yes, regular pelvic floor exercises can significantly improve bladder control by strengthening the muscles that support the bladder and other pelvic organs. These exercises are particularly effective when performed correctly and consistently.
Is local vaginal estrogen therapy safe and beneficial for overactive bladder caused by menopause?
Local vaginal estrogen therapy is generally safe and effective for treating overactive bladder symptoms during menopause. It helps restore urinary tract tissue health with minimal systemic absorption, though individual suitability should be discussed with a healthcare provider.
What lifestyle changes can help prevent or reduce overactive bladder symptoms during menopause?
Key lifestyle changes include maintaining a healthy weight, limiting bladder irritants like caffeine and alcohol, practicing timed voiding, staying physically active, and managing fluid intake. Keeping a bladder diary can also help identify triggers and track improvement.