Pancolitis represents a severe form of ulcerative colitis that affects the entire colon, causing widespread inflammation and potentially serious complications. Understanding this condition is crucial for proper management and improved quality of life for those affected. This comprehensive guide explores the key aspects of pancolitis, from recognizing symptoms to exploring various treatment approaches.
Understanding Pancolitis and Its Impact
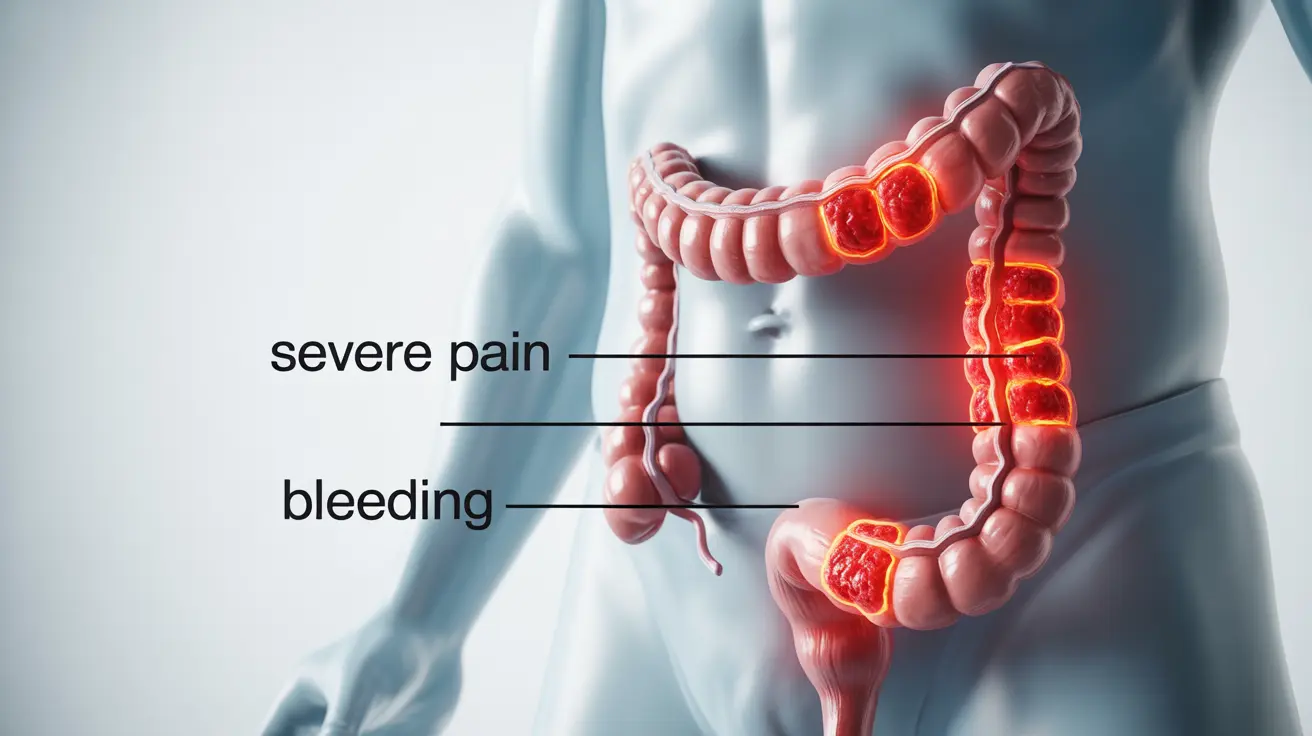
Pancolitis differs from other forms of ulcerative colitis primarily in its extent, affecting the entire large intestine from the rectum to the cecum. This extensive inflammation can lead to more severe symptoms and complications compared to limited forms of ulcerative colitis, making early detection and proper management essential.
Key Symptoms and Warning Signs
The symptoms of pancolitis tend to be more severe and widespread than other forms of ulcerative colitis. Common indicators include:
- Frequent bloody diarrhea
- Severe abdominal pain and cramping
- Significant weight loss
- Extreme fatigue
- Fever in some cases
- Night sweats
- Loss of appetite
Diagnostic Process and Testing
Diagnosing pancolitis requires a comprehensive medical evaluation and several specific tests:
Physical Examination and Medical History
Your healthcare provider will begin with a detailed discussion of your symptoms and medical history, followed by a physical examination to check for signs of inflammation and complications.
Diagnostic Tests
- Colonoscopy with biopsy
- Blood tests to check for inflammation markers
- Stool samples
- Imaging studies (CT scan or MRI) when necessary
Treatment Approaches
Medical Management
Treatment typically follows a step-up approach, starting with less aggressive options and escalating as needed:
- Anti-inflammatory medications
- Immunosuppressants
- Biological therapies
- Corticosteroids for severe flares
Lifestyle Modifications
Several lifestyle changes can help manage symptoms and reduce flare-ups:
- Dietary modifications
- Stress management techniques
- Regular exercise when appropriate
- Adequate rest and sleep
- Smoking cessation
Surgical Intervention
In some cases, surgery becomes necessary when medical management fails or complications develop. The most common surgical procedure is total proctocolectomy with ileal pouch-anal anastomosis (IPAA), which removes the entire colon while preserving bowel function.
Frequently Asked Questions
1. What are the main symptoms that indicate pancolitis versus other forms of ulcerative colitis?
Pancolitis symptoms tend to be more severe and widespread, including frequent bloody diarrhea, severe abdominal pain throughout the entire colon, significant weight loss, and extreme fatigue. Unlike limited forms of ulcerative colitis, these symptoms affect the entire large intestine.
2. How is pancolitis diagnosed and what tests are commonly used?
Diagnosis typically involves a combination of colonoscopy with biopsy, blood tests, stool samples, and imaging studies. The colonoscopy is particularly important as it allows doctors to visualize the extent of inflammation throughout the entire colon.
3. What treatment options are available for managing pancolitis and how do doctors decide which to use?
Treatment options range from anti-inflammatory medications to immunosuppressants and biologics. Doctors base their decisions on disease severity, previous treatment responses, and individual patient factors. They typically follow a step-up approach, starting with less aggressive treatments and escalating as needed.
4. Can lifestyle changes or natural remedies help reduce pancolitis flare-ups?
Yes, lifestyle modifications can help manage symptoms. These include dietary changes, stress management, regular exercise, and adequate rest. However, these should complement, not replace, medical treatment.
5. When is surgery necessary for pancolitis, and what does the procedure involve?
Surgery becomes necessary when medical treatments fail to control symptoms, complications develop, or there's a high risk of colorectal cancer. The standard procedure is total proctocolectomy with IPAA, which removes the entire colon and creates a new way for waste to leave the body.