The pancreas plays a crucial role in maintaining healthy blood sugar levels through insulin production, but various factors can disrupt this vital function. When the pancreas stops producing adequate insulin or becomes ineffective at releasing it, diabetes develops, affecting millions of people worldwide. Understanding the underlying mechanisms behind pancreatic dysfunction is essential for managing and preventing this chronic condition.
Insulin production failure doesn't happen overnight and involves complex biological processes that differ between type 1 and type 2 diabetes. Recognizing the early warning signs and understanding the root causes can help individuals take proactive steps toward better pancreatic health and diabetes prevention.
The Pancreas and Insulin Production
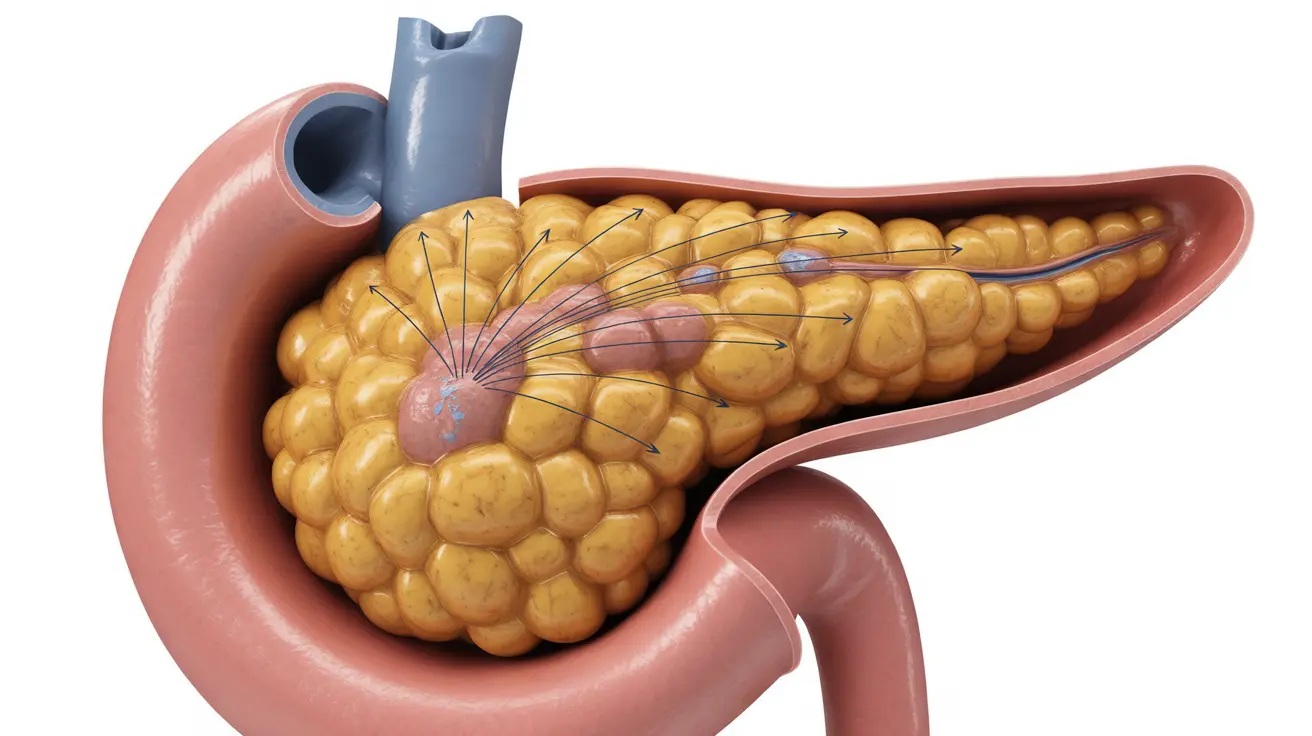
The pancreas contains specialized clusters of cells called islets of Langerhans, which house beta cells responsible for insulin production. These beta cells constantly monitor blood glucose levels and release insulin accordingly to help cells absorb sugar for energy or storage. When this delicate system becomes compromised, blood sugar levels rise uncontrollably.
Healthy beta cells can adjust insulin production based on the body's needs, increasing output after meals and reducing it during fasting periods. However, various factors can damage or destroy these cells, leading to insufficient insulin production and the development of diabetes.
Type 1 Diabetes: Autoimmune Destruction of Beta Cells
In type 1 diabetes, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This autoimmune response typically occurs due to a combination of genetic predisposition and environmental triggers, such as viral infections or exposure to certain toxins.
The destruction process can take months or years to complete, but once a significant percentage of beta cells are destroyed, insulin production drops dramatically. Unlike type 2 diabetes, this damage is usually irreversible, requiring lifelong insulin replacement therapy.
Genetic markers and family history play significant roles in type 1 diabetes development, though environmental factors often serve as the final trigger that activates the autoimmune response against pancreatic beta cells.
Type 2 Diabetes: Progressive Beta Cell Dysfunction
Type 2 diabetes involves a more gradual process where beta cells become overworked and eventually fail to produce sufficient insulin. Initially, the pancreas may actually produce more insulin than normal to compensate for insulin resistance in muscle, liver, and fat cells.
Over time, this increased demand exhausts the beta cells, leading to decreased insulin production. Factors contributing to this process include obesity, sedentary lifestyle, poor diet, chronic inflammation, and genetic predisposition. The progression from normal glucose tolerance to full-blown diabetes can span several years.
Unlike type 1 diabetes, type 2 diabetes often develops alongside insulin resistance, where cells become less responsive to insulin's effects, creating a dual problem of both reduced insulin sensitivity and eventual production decline.
Lifestyle Factors and Pancreatic Health
Several lifestyle factors directly impact pancreatic function and insulin production capacity. Chronic overeating, particularly foods high in refined sugars and processed carbohydrates, forces beta cells to work overtime, potentially leading to burnout and decreased function over time.
Physical inactivity contributes to insulin resistance, requiring the pancreas to produce more insulin to maintain normal blood sugar levels. Regular exercise improves insulin sensitivity, reducing the workload on pancreatic beta cells and helping preserve their function.
Obesity, especially abdominal fat accumulation, creates chronic low-grade inflammation that can damage beta cells and impair insulin production. Maintaining a healthy weight through proper nutrition and regular physical activity supports optimal pancreatic function.
Medical Conditions Affecting Insulin Production
Several medical conditions can directly damage the pancreas and impair insulin production. Pancreatitis, both acute and chronic forms, causes inflammation that can destroy insulin-producing cells. Repeated episodes of pancreatitis significantly increase diabetes risk due to cumulative pancreatic damage.
Pancreatic cancer can destroy healthy tissue, including beta cells, leading to diabetes development. In some cases, new-onset diabetes in older adults may be an early warning sign of pancreatic cancer, highlighting the importance of proper medical evaluation.
Other conditions such as cystic fibrosis, hemochromatosis, and certain medications can also impair pancreatic function and insulin production, leading to secondary forms of diabetes that require specialized management approaches.
Recognizing Early Warning Signs
Early signs of declining insulin production include persistent fatigue, increased thirst, frequent urination, and unexplained weight loss. These symptoms develop gradually and may be attributed to other causes initially, delaying proper diagnosis and treatment.
Changes in appetite, slow-healing wounds, and recurrent infections can also indicate inadequate insulin production. Blurred vision and tingling in hands or feet may signal that blood sugar levels have been elevated for an extended period.
Regular health screenings, including blood glucose tests, can detect declining pancreatic function before symptoms become severe. Early intervention can help preserve remaining beta cell function and prevent complications.
Frequently Asked Questions
What causes the pancreas to stop producing insulin in type 1 and type 2 diabetes?
In type 1 diabetes, an autoimmune response destroys insulin-producing beta cells, typically triggered by genetic factors combined with environmental influences like infections. Type 2 diabetes develops when beta cells become overworked due to insulin resistance and lifestyle factors, eventually leading to decreased insulin production over time.
Can lifestyle changes help the pancreas produce more insulin in type 2 diabetes?
Yes, lifestyle modifications can help preserve and potentially improve pancreatic function in type 2 diabetes. Regular exercise increases insulin sensitivity, reducing the workload on beta cells. A healthy diet with controlled portions and limited processed foods prevents excessive strain on the pancreas. Weight loss, particularly reducing abdominal fat, can significantly improve beta cell function and insulin production.
What are the early signs that the pancreas is not producing enough insulin?
Early warning signs include increased thirst, frequent urination, persistent fatigue, and unexplained weight loss. Additional symptoms may include changes in appetite, slow wound healing, recurrent infections, blurred vision, and tingling in extremities. These symptoms often develop gradually and may be subtle initially.
How does insulin resistance lead to the pancreas failing to produce insulin?
Insulin resistance forces the pancreas to produce increasingly larger amounts of insulin to maintain normal blood sugar levels. This increased demand overworks the beta cells, causing them to become exhausted and eventually fail. The progression from insulin resistance to beta cell failure typically occurs over several years, with the pancreas initially compensating through increased production before eventually declining.
Can pancreatitis or pancreatic cancer affect insulin production and cause diabetes?
Yes, both conditions can significantly impact insulin production. Pancreatitis causes inflammation that damages insulin-producing beta cells, with chronic or repeated episodes increasing diabetes risk substantially. Pancreatic cancer destroys healthy pancreatic tissue, including beta cells, and new-onset diabetes in older adults may sometimes be an early indicator of pancreatic malignancy requiring immediate medical evaluation.